Effect on gut microbiome emerges as another benefit of statin therapy
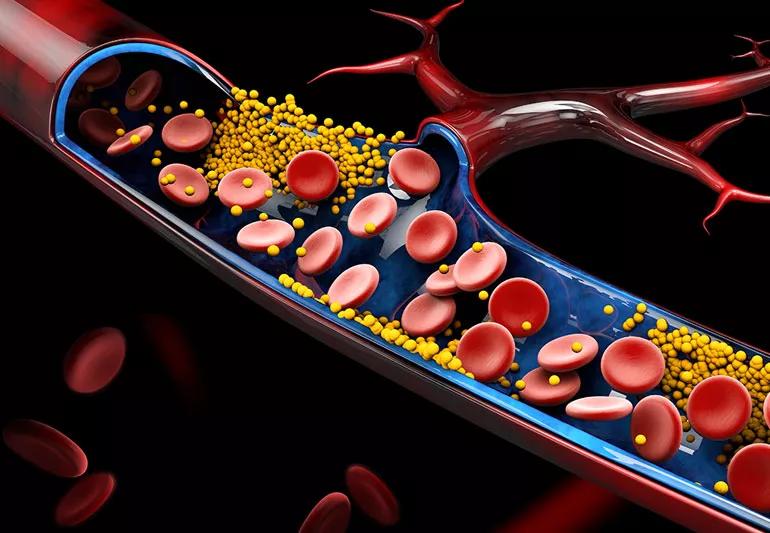
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/98cfc4be-5d39-44f3-9134-6b7710deaf6d/plaqueBloodVessel-1159729392_770x533_jpg)
Statins
Statin therapy significantly reduces plasma levels of trimethylamine N-oxide (TMAO), an atherogenic metabolite produced by gut bacteria. This finding, from the largest study to date of a statin drug’s effects on plasma TMAO levels, suggests an additional mechanism of cardiovascular benefit conferred by statin drugs besides improving lipid profiles and attenuating inflammation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Cleveland Clinic-led study, published in the American Journal of Cardiology (2022;178:26-34), analyzed three independent patient cohorts and included more than 1,000 propensity-matched pairs of subjects who were either treated or not treated with statins.
“Our findings support an explanation for observed cardiovascular benefits of statin therapy beyond well-established effects,” says corresponding author W.H. Wilson Tang, MD, Research Director in Cleveland Clinic’s Section of Heart Failure and Cardiac Transplantation Medicine. “They suggest the possibility that TMAO levels can be used to further stratify cardiovascular risk when characterizing patient response to statins.”
Dr. Tang is part of a Cleveland Clinic team led by Stanley Hazen, MD, PhD, that has conducted multiple investigations on the role of TMAO, a metabolite produced from digestion by gut bacteria of choline, carnitine and lecithin — nutrients that are particularly abundant in animal products, especially red meat. Animal and clinical association studies have linked elevated levels of TMAO to atherosclerosis, thrombosis and other cardiometabolic diseases.
The research team recently turned its attention to statins. Increasing evidence suggests statin therapy affects the gut microbiome, although the precise impacts and mechanisms are only beginning to be explored. “Better understanding of the nature of statin-induced changes may help explain why heterogeneity exists in individual responses to statin therapy,” says Dr. Hazen, Co-Section Head of Preventive Cardiology and Rehabilitation.
Advertisement
The current investigation made use of subjects from the following studies:
The investigators analyzed TMAO levels of available fasting blood samples from the IMI and AARG study cohorts.
Propensity score matching with multiple variables (including demographics, comorbidities, baseline lab measures and medications) was applied to the GeneBank study cohort to establish 1,196 matched pairs of patients who either were or were not using statins.
The IMI and AARG study cohorts allowed investigation of the effect of statin use on blood TMAO levels. Among the key findings:
Advertisement
Among the GeneBank matched pairs, patients taking statins had lower plasma TMAO than those not on statins (P = 0.002). Over the follow-up period, 322 patients in total experienced a major adverse cardiovascular event. Among the matched cohort:
“Interestingly, there was minimal correlation between TMAO and cholesterol levels when they were directly compared,” Dr. Tang notes.
In their study report, the investigators, led by co-first authors Daniel Li, MD, and Xinmin Li, PhD, underscore the following key conclusions:
“People with a high baseline TMAO level may represent a subgroup of patients who are likelier to derive significant benefit from statin therapy,” Dr. Tang says.
The authors discuss possible mechanisms by which statins may result in TMAO reductions, including direct statin-gut microbiome interactions and changes in cholesterol metabolism, bile acid composition, inflammation and gut permeability.
Advertisement
“This study highlights the gut-cardiovascular axis as a possible important contributor to cardiovascular risk,” Dr. Hazen observes. “It opens up new avenues of investigation into the role of the microbiome in cardiovascular disease.”
Advertisement
Advertisement
Phase 3 TANDEM study may help pave way to first approval of a CETP inhibitor
Reassurance from the lipid outcomes trial with the highest percentage female enrollment to date
Tech-assisted self-selection concurred with clinician-assessed eligibility in >90% of cases
Robust reductions in cardiac events seen in high-risk patients without prior events
Findings bolster the oral drug as an option for primary and secondary prevention
Randomized controlled study undercuts unsubstantiated ‘heart health’ claims
First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3
Cleveland Clinic pioneers a new paradigm in cardiovascular care delivery