Phase 3 TANDEM study may help pave way to first approval of a CETP inhibitor
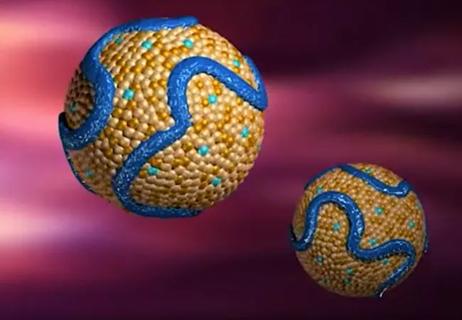
A fixed-dose oral combination of the CETP inhibitor obicetrapib and ezetimibe lowered LDL cholesterol (LDL-C) levels by nearly 50% at 12 weeks compared with placebo in patients with or at high risk for atherosclerotic cardiovascular disease (ASCVD) in the phase 3 TANDEM study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is the first phase 3 trial evaluating the LDL cholesterol-lowering efficacy of a combination of this investigational CETP inhibitor with the established lipid-lowering drug ezetimibe in the setting of ASCVD,” says the study’s first author, Ashish Sarraju, MD, a Cleveland Clinic cardiologist who served as principal investigator. The TANDEM results were presented by Cleveland Clinic’s Steven Nissen, MD, chair of the trial’s executive steering committee, at the European Atherosclerosis Society Congress in Glasgow. They were simultaneously published in The Lancet.
“TANDEM showed that this fixed-dose combination reduced LDL cholesterol significantly more than either of its component drugs alone, with good overall tolerance,” Dr. Sarraju adds. “It achieved a degree of LDL cholesterol reduction similar to high-intensity statin therapy and approaching that of PCSK9 inhibitors.
“There is increasing recognition of the power of combination therapy for lipid lowering,” he continues. “If ultimately approved, this single-pill combination therapy could offer another option for quickly reducing LDL cholesterol to very low levels in high-risk patients, who sometimes can be challenging to treat.”
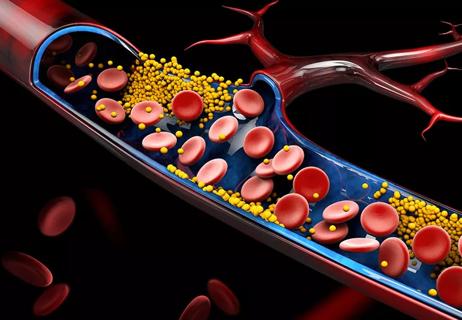
Many patients at high risk for ASCVD events do not reach target levels of LDL-C after use of maximally tolerated statin therapy. Injectable medications are available for LDL-C reduction in this setting, but some patients are wary of injectables and others have limited insurance access to them. While some non-statin oral therapies are available, considerable numbers of patients continue to fall short of their LDL-C reduction targets.
Advertisement
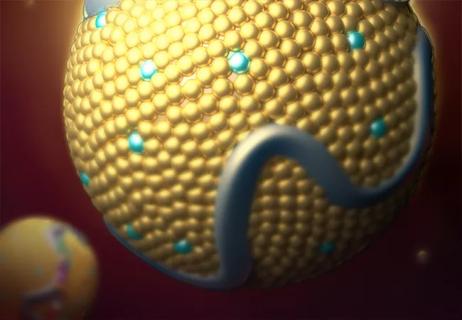
CETP inhibitors have long been studied as a potential additional oral option for treating ASCVD, but four prior CETP inhibitor candidates have not achieved success in clinical trials. Initial trials focused on the ability of this class to raise HDL cholesterol levels, but neither these trials nor later studies focusing on LDL-C reduction yielded sufficiently positive overall efficacy results. One CETP inhibitor was abandoned due to an association with increased systolic blood pressure.
Obicetrapib is a newer selective CETP inhibitor that has been shown to significantly lower LDL-C in small phase 2 studies when given as monotherapy or in combination with ezetimibe to patients without ASCVD. TANDEM (NCT06005597) was undertaken to assess the combination of obicetrapib and ezetimibe in a larger number of patients with preexisting ASCVD or high risk for it.
TANDEM researchers randomized 407 adults across 48 U.S. sites, including Cleveland Clinic. Participants had or were at risk for ASCVD and/or had heterozygous familial hypercholesterolemia; all had LDL-C levels ≥ 70 mg/dL (≥ 1.8 mmol/L) despite maximally tolerated lipid-lowering therapy (excluding ezetimibe), and all were required to be receiving maximally tolerated statin therapy or to have documented statin intolerance.
Patients (median age, 68 years; 43.5% female) were randomized in double-blind fashion to 12 weeks of once-daily therapy with one of the following:
Advertisement
Primary endpoints were the percentage change in LDL-C in the FDC group relative to the other groups, as well as the placebo-adjusted change in the obicetrapib monotherapy group.
After 12 weeks, the differences in LDL-C reduction between the FDC group and the other groups were as follows:
On the other co-primary endpoint, obicetrapib monotherapy reduced LDL-C by 31.9% (95% CI, 22.9% to 41.6%) relative to placebo.
Rates of adverse events are detailed in the table below. The incidence of any adverse event was lowest in the placebo group and generally comparable between the FDC group and the two monotherapy groups. Rates of serious adverse events and adverse events leading to therapy discontinuation were broadly similar between the FDC group and all other groups. Prespecified events (including changes in systolic blood pressure) and lab findings of particular interest were not meaningfully different between the FDC and monotherapy groups.
| Fixed-dose combination | Obicetrapib | Ezetimibe | Placebo | |
|---|---|---|---|---|
| Any adverse event | 51% | 54% | 53% | 37% |
| Adverse event leading to discontinuation of trial agent | 5% | 9% | 7% | 4% |
| Serious adverse event | 3% | 6% | 7% | 4% |
| Any adverse event | ||||
| Fixed-dose combination | ||||
| 51% | ||||
| Obicetrapib | ||||
| 54% | ||||
| Ezetimibe | ||||
| 53% | ||||
| Placebo | ||||
| 37% | ||||
| Adverse event leading to discontinuation of trial agent | ||||
| Fixed-dose combination | ||||
| 5% | ||||
| Obicetrapib | ||||
| 9% | ||||
| Ezetimibe | ||||
| 7% | ||||
| Placebo | ||||
| 4% | ||||
| Serious adverse event | ||||
| Fixed-dose combination | ||||
| 3% | ||||
| Obicetrapib | ||||
| 6% | ||||
| Ezetimibe | ||||
| 7% | ||||
| Placebo | ||||
| 4% |
Other findings of interest:
Advertisement
“These findings suggest that, if approved for clinical use, the fixed-dose combination of obicetrapib and ezetimibe may be a useful option as an adjunct to statin therapy for patients with or at high risk for ASCVD who have intolerance to or inadequate response to existing therapies,” Dr. Sarraju observes.
“Many experts now recommend starting treatment with combination therapies rather than try a single medication and adding additional therapies later,” adds Dr. Nissen, senior author of the study and Chief Academic Officer of Cleveland Clinic’s Heart, Vascular and Thoracic Institute. “This strategy gets more patients to goal more quickly and makes good sense for high-risk patients.”
Dr. Sarraju says the TANDEM results may support a regulatory filing for this fixed-dose combination therapy for an LDL-C reduction indication. Meanwhile, investigation of obicetrapib monotherapy continues in PREVAIL, a fully enrolled large cardiovascular outcome trial that will determine whether the drug’s lipid-lowering effects translate to a reduction of major adverse cardiovascular events.
Dr. Sarraju is hopeful that an eventual approval of obicetrapib — in combination with ezetimibe and/or as a stand-alone pill — would benefit patients through expanded options. “The key with lipid lowering is getting patients to their LDL cholesterol goal as quickly as possible in a manner that they’re comfortable with and they tolerate,” he says. “The more options we can offer to patients to make a therapeutic decision that suits them well, the greater the chance of reducing their cardiovascular risk.”
Advertisement
Leslie Cho, MD, Section Head of Preventive Cardiology at Cleveland Clinic, concurs. “I am glad to see the field of cholesterol-lowering medications continue to grow, giving patients more options,” she says. “Hopefully this will translate to lowering the cost of medications. We await the cardiovascular outcome trial for obicetrapib.”
For more on the TANDEM trial and its implications, check out this recent 9-minute episode of Cleveland Clinic's Cardiac Consult podcast featuring Drs. Sarraju and Nissen.
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2237537/17562768)
Advertisement

Reassurance from the lipid outcomes trial with the highest percentage female enrollment to date

Tech-assisted self-selection concurred with clinician-assessed eligibility in >90% of cases
Robust reductions in cardiac events seen in high-risk patients without prior events
Findings bolster the oral drug as an option for primary and secondary prevention
Effect on gut microbiome emerges as another benefit of statin therapy

Randomized controlled study undercuts unsubstantiated ‘heart health’ claims

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Yet 21.4% of tested individuals had Lp(a) elevation