Yet 21.4% of tested individuals had Lp(a) elevation
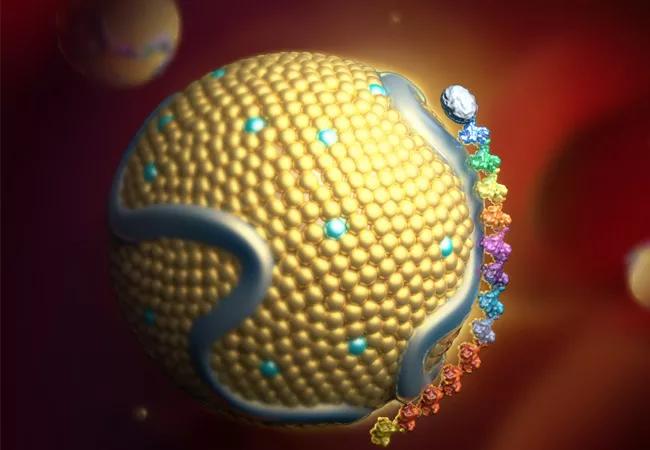
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5ebc3a29-54ae-4a22-9925-6cb5fc792547/22-HVI-2769711_lipoproteina_650x450-jpg)
lipoprotein(a) particle
Just 0.1% of adults in a contemporary cohort of 71 million individuals from the general population had ever undergone lipoprotein(a) (Lp(a)) testing, finds a new study by Cleveland Clinic researchers published in Circulation. Yet among those whose Lp(a) was tested, the prevalence of Lp(a) elevation was 21.4% — and considerably higher in selected at-risk subgroups.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Despite guidelines recommending Lp(a) measurement, our findings reveal striking underutilization of this important cardiovascular risk marker,” says the study’s senior and corresponding author, Leslie Cho, MD, Co-Section Head of Preventive Cardiology at Cleveland Clinic. “Even in high-risk populations where testing would be most beneficial, the rates remain very low.”
Guidelines from the European Society of Cardiology recommend one-time measurement of Lp(a) in all adults to help in evaluating cardiovascular risk. The American College of Cardiology and American Heart Association advocate consideration of Lp(a) testing for adults with personal or family history of atherosclerotic disease (ASCVD) that is not fully explained by major CVD risk factors.
Prior reports of low utilization of Lp(a) testing despite these recommendations prompted the current retrospective, observational study by Dr. Cho and a Cleveland Clinic colleague. They examined a large cohort of patients using the TriNetX Analytics Research Network database to determine the prevalence of Lp(a) testing between January 2015 and March 2024. Data on individuals undergoing Lp(a) testing were obtained from 48 healthcare organizations participating in the database, 43 of which were in the U.S.
Prevalence of Lp(a) testing was assessed among the overall cohort of adult patients and various subgroups of interest, as detailed in the table below.
| Group | Prevalence of Lp(a) testing |
|---|---|
| All adults in the cohort (n = 70,820,858) | 0.10% |
| Those with premature ASCVD (n = 1,670,459) | 0.75% |
| Those with familial hypercholesterolemia (n = 102,954) | 3.52% |
| Those with aortic stenosis (n = 711,504) | 0.42% |
| Those ≤50 years with acute myocardial infarction (n = 362,681) | 0.85% |
| Those ≤50 years with ST-elevation myocardial infarction (n = 67,439) | 1.16% |
| Those with family history of ASCVD (n = 3,259,889) | 0.19% |
| Group | |
| All adults in the cohort (n = 70,820,858) | |
| Prevalence of Lp(a) testing | |
| 0.10% | |
| Those with premature ASCVD (n = 1,670,459) | |
| Prevalence of Lp(a) testing | |
| 0.75% | |
| Those with familial hypercholesterolemia (n = 102,954) | |
| Prevalence of Lp(a) testing | |
| 3.52% | |
| Those with aortic stenosis (n = 711,504) | |
| Prevalence of Lp(a) testing | |
| 0.42% | |
| Those ≤50 years with acute myocardial infarction (n = 362,681) | |
| Prevalence of Lp(a) testing | |
| 0.85% | |
| Those ≤50 years with ST-elevation myocardial infarction (n = 67,439) | |
| Prevalence of Lp(a) testing | |
| 1.16% | |
| Those with family history of ASCVD (n = 3,259,889) | |
| Prevalence of Lp(a) testing | |
| 0.19% |
Among patients who were tested, the prevalence of an elevated Lp(a) level (i.e., ≥50 mg/dL or ≥125 nmol/L) was high, as detailed in the table below.
Advertisement
| Group of tested individuals | Prevalence elevated Lp(a) |
|---|---|
| Overall cohort (n = 70,976) | 21.4% |
| Those with premature ASCVD (n = 12,456) | 36.3% |
| Those with familial hypercholesterolemia (n = 3,624) | 40.7% |
| Those with aortic stenosis (n = 2,942) | 37.1% |
| Those ≤50 years with acute myocardial infarction (n = 3,072) | 40.1% |
| Those with family history of ASCVD (n = 6,034) | 24.1% |
| Group of tested individuals | |
| Overall cohort (n = 70,976) | |
| Prevalence elevated Lp(a) | |
| 21.4% | |
| Those with premature ASCVD (n = 12,456) | |
| Prevalence elevated Lp(a) | |
| 36.3% | |
| Those with familial hypercholesterolemia (n = 3,624) | |
| Prevalence elevated Lp(a) | |
| 40.7% | |
| Those with aortic stenosis (n = 2,942) | |
| Prevalence elevated Lp(a) | |
| 37.1% | |
| Those ≤50 years with acute myocardial infarction (n = 3,072) | |
| Prevalence elevated Lp(a) | |
| 40.1% | |
| Those with family history of ASCVD (n = 6,034) | |
| Prevalence elevated Lp(a) | |
| 24.1% |
The researchers did note a positive trend in testing frequency over time, with annual testing numbers increasing from 1,690 in 2015 to 20,817 in 2023 (P < .001). “Despite this modest progress, the overall prevalence remains dramatically below what guidelines suggest is optimal,” Dr. Cho notes.
Demographic analysis of patients who underwent testing showed a mean age of 58.4 years, with an essentially 50/50 sex distribution. Black patients were less likely to undergo Lp(a) testing compared with other racial groups (P < .001).
The study authors identify several barriers hindering more widespread Lp(a) testing, including lack of awareness about Lp(a)’s role in cardiovascular disease, unclear testing guidelines, inadequate treatment strategies for patients with Lp(a) elevation, the absence of testing programs, variability in clinical assays and lack of coverage by insurers. To address the latter, the authors recommend that clinicians present payors with recent evidence and guidelines demonstrating the cost-effectiveness and clinical utility of Lp(a) testing and emphasize the numerous promising therapies in development to reduce Lp(a).
“It is a shame that so few patients are getting tested for Lp(a),” says Dr. Cho, “as it is a causal risk factor for premature coronary artery disease, myocardial infarction, stroke and calcific aortic stenosis. European, British, Canadian, Japanese, Australian and Indian guidelines all recommend testing at least once in patient’s lifetime. It is imperative that we start testing in the U.S.”
Advertisement
“Cardiovascular outcome trials of therapies that reduce lipoprotein(a) will complete within the next year or two,” adds Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular and Thoracic Institute. “If these trials are successful in reducing major cardiovascular events, we need to know whom to treat. Undertesting will prevent millions of patients who might benefit from these new drugs from receiving treatment. It’s a major public health problem.”
Advertisement
Advertisement
Small interfering RNA lowered lipoprotein(a) by 94% during six-month follow-up after a single dose
Phase 2 trial of zerlasiran yields first demonstration of longer effect with each dose of an siRNA
It's time to increase testing for this major cardiovascular risk factor in advance of new therapies
Undetectable levels achieved for nearly nine months in phase 1 trial
First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3
Proteins related to altered immune response are potential biomarkers of the rare AD variant
Phase 3 TANDEM study may help pave way to first approval of a CETP inhibitor
Resourceful approaches to the care of patients with microvascular disease and elevated Lp(a)