Dr. Jeffrey Cohen on the challenges that temper the promise
Stem cell therapies offer a promising approach for immunomodulation, neuroprotection and repair of damaged nervous systems, but they are not yet ready for prime time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So argued Jeffrey A. Cohen, MD, Director of Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, at an April 25 “Section Topic Controversies” session on stem cell therapies for neurological diseases at the American Academy of Neurology’s 2017 annual meeting in Boston. In a talk titled “The Devilish Details, Challenges and Uncertainties,” Dr. Cohen presented the more cautionary side of the debate.
“Many stem cell therapies are in various stages of development, each with its own purpose, datasets, risks and efficacies,” Dr. Cohen said. “None should be considered standard care at this time.”
Most of the session centered on two approaches (summarized below) that have received the most attention for multiple sclerosis (MS), a disease on which Dr. Cohen has published and presented at international conferences. He emphasized, however, that the concepts debated are generally applicable to other stem cell therapies and for other neurological diseases, including Parkinson’s disease, Huntington’s disease and traumatic brain injury.
Immunoablation followed by infusion of autologous HSCs can be viewed as a potent anti-inflammatory strategy for rebooting the immune system. Evidence to date shows that the therapy is long-lasting, based on up to seven years’ worth of longitudinal data in patients with MS.
But Dr. Cohen, who also serves as Director of Cleveland Clinic’s Experimental Therapeutics Program, advised caution to his colleagues before they consider offering this therapy, for the following reasons:
Advertisement
Stem cells can be recruited to repair damaged nervous tissue, offering an exciting potential avenue of therapy for patients with progressive forms of MS as well as other conditions in which neural injury has occurred.
Dr. Cohen, who has been involved in early-phase studies of repair-promoting stem cell therapies, emphasized that such therapies are still in the experimental stages for MS and other neurological diseases, and it is premature to offer them in clinical practice. Although some safety studies have been completed with good results, the therapies’ benefits have yet to be proven in clinical trials.
The lack of evidence for efficacy has not stopped some freestanding clinics from offering this therapy directly to patients who are desperate for an alternative treatment option and willing to try “medical tourism.” As for all clinical cell-based therapies, rigorous quality and safety control in cell production is critical, which makes seeking treatment from commercial clinics in countries where medical facilities might be poorly regulated especially worrisome.
Dr. Cohen touched on some fundamental questions that have yet to be answered:
Advertisement
“It can be argued that it’s even too early to have clinical trials on these therapies,” Dr. Cohen cautioned. “No one really knows how these treatments should be performed.”
Cell-based treatments for neurological diseases are now in various phases of clinical trials and offer high hopes of potential benefits for disease-modifying and restorative therapy, Dr. Cohen concluded. He added, however, that much work remains in defining their therapeutic roles relative to existing therapies, identifying appropriate candidate populations and sorting out the logistics of a new treatment paradigm.
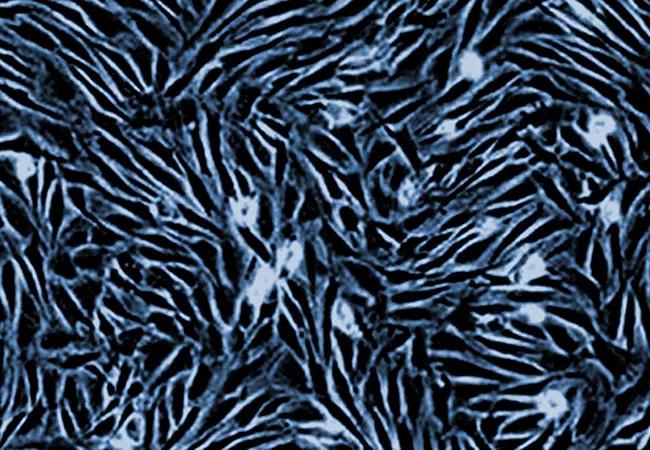
Image at top: Characteristic morphology of mesenchymal stem cells in culture.
Advertisement
Advertisement

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant