One-year stroke mortality rate down by 18 percent over five years
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
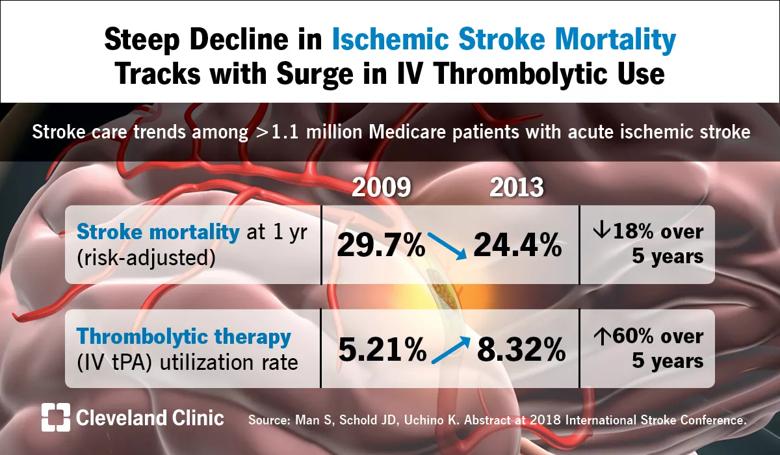
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd943e6c-f72a-41e6-bed6-f2fd7962c528/18-NEU-547-Stroke-Visual-Abstract-FNL_jpg)
From 2009 to 2013, case fatality rates during the year after an ischemic stroke declined by 18 percent among Medicare beneficiaries, and the improvement was mirrored by a 60 percent rise in the use of intravenous (IV) thrombolytic therapy over the same period. So finds a Cleveland Clinic-led analysis of more than 1.1 million Medicare beneficiaries presented at the 2018 International Stroke Conference (ISC 2018) in Los Angeles.
Deaths from stroke have been decreasing for decades in adults in the U.S. and many European countries. While early gains have been mainly attributable to improved control and prevention of vascular risk factors, this study sought to determine the reasons for continuing declines in mortality in recent years.
“Stroke mortality trends have been going in the right direction despite increasing prevalence of comorbidities in patients,” says Ken Uchino, MD, the study’s senior author and Director of Research and Education for Cleveland Clinic’s Cerebrovascular Center. “Our findings confirm that IV thrombolytic therapy is an important part of the positive trends.”
Data were analyzed from the Medicare Provider Analysis and Review national database of beneficiaries aged 65 or over who were hospitalized between January 1, 2009, and December 31, 2013, with a primary discharge diagnosis of acute ischemic stroke. The study included 1,165,960 patients.
Main outcomes of interest were risk-adjusted one-year mortality, use of IV thrombolytic therapy (tissue plasminogen activator [tPA]) and the relation between the two. Cox proportional hazards modeling was done to adjust for patient demographics and comorbidities.
Advertisement
Among the key findings:
The above mortality improvements were achieved despite an increase in the prevalence of comorbidities among ischemic stroke patients, especially hypertension, atrial fibrillation, prior cerebrovascular disease, chronic obstructive pulmonary disease, renal failure and diabetes.
Moreover, although increasing use of proven therapies would be expected to correspond with improved death rates, the reason behind the steady improvement in thrombolytic therapy use throughout the study period is unclear, since IV tPA had been available for many years before 2009.
Advertisement
Although the available data do not provide an answer, Dr. Uchino says several possibilities come to mind. First, patterns of thrombolytic treatment have changed over time, with earlier administration of IV tPA after symptom onset, better post-tPA management, or increasing treatment of milder strokes, transient ischemic attacks and stroke mimics.
Additionally, general stroke care quality has improved, with increasing use of thrombectomy, enhanced quality in admissions and hospital care, and better prevention of complications and secondary strokes. Although these general improvements should be seen across the board in IV tPA recipients and nonrecipients alike, it’s possible that they were more available in hospitals that made optimal use of IV tPA therapy, Dr. Uchino speculates.
Testing such hypotheses will take more delving into the data, he adds. “As more Medicare data become available, we will continue to analyze trends to learn what we can with the goal of improving patient care,” he concludes.
The study was presented at ISC 2018 by Shumei Man, MD, PhD, Wright State University Boonshoft School of Medicine in Dayton, Ohio, who was a vascular neurology fellow at Cleveland Clinic when this research was conducted. The other co-author, Jesse Schold, PhD, is a biostatistician with Cleveland Clinic. The study was supported by a grant from the American Heart Association.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help