Suspected factors include antithrombotic intensity, time on device, presence of thrombocytopenia
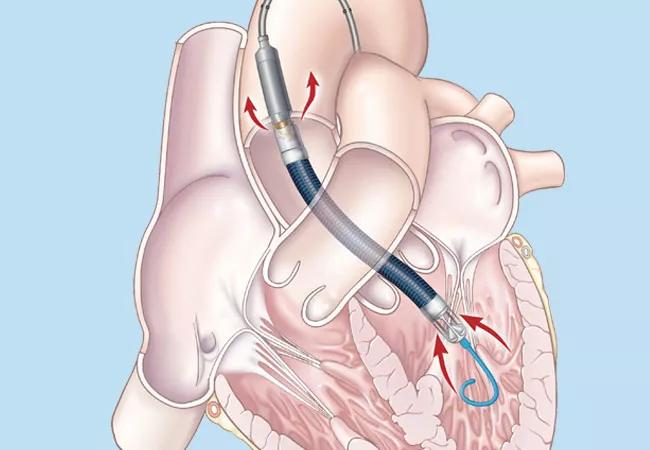
For patients on short-term cardiac support with an Impella device, inadequate anticoagulation, duration of cardiac support and a low platelet count all may play roles in causing an ischemic stroke or intracranial hemorrhage. So finds a newly published single-institution series from Cleveland Clinic (ASAIO J. 2020;66[8]:e105-e109) analyzing outcomes among 79 patients with acute cardiogenic shock who underwent implantation of Impella, a percutaneously placed temporary left ventricular assist device (LVAD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ischemic stroke and intracranial hemorrhage are common causes of death and disability in patients who receive a long-term implantable LVAD, with many of these events occurring perioperatively. But the incidence of, and risk factors for, acute neurologic events in patients on short-term cardiac support with a percutaneous temporary LVAD have not been well characterized.
“Causes of these devastating acute neurologic events with short-term Impella support have not been thoroughly explored,” says stroke neurologist Ken Uchino, MD, the study’s senior and corresponding author and Head of Research and Education in Cleveland Clinic’s Cerebrovascular Center. “Our case series revealed plausible risk factors and sets the stage for further investigation.”
Dr. Uchino and colleagues reviewed prospectively collected data on 79 consecutive patients implanted with an Impella device (Impella 2.5, 5.0, CP or RP) at Cleveland Clinic between October 2010 and July 2018. The median duration of Impella support was 8 days (range, 1-33).
Six patients (7.5%) were found to have had an acute neurologic event, as follows:
Of these six patients, four died during hospitalization, and the other two survived to heart transplantation (one underwent transplant the day before the acute neurologic event). Analysis of the six patients revealed the following:
Advertisement
The incidence of ischemic or hemorrhagic stroke in this series (7.5%) was higher than in other published studies, which found a less than 2% incidence during the implantation period. The researchers note that while the reasons for this difference cannot be answered by this study, their findings focus attention on several key questions:
Advertisement
“This small retrospective study cannot determine the exact cause of neurologic events in Impella-treated cardiogenic shock patients, a population with a high risk of stroke and many confounding factors,” concludes Dr. Uchino. “But it does highlight a number of issues that will be helpful to explore in larger randomized controlled trials and prospective studies.”
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits