For the first time, risk is shown after accounting for underlying contributions of pulmonary disease
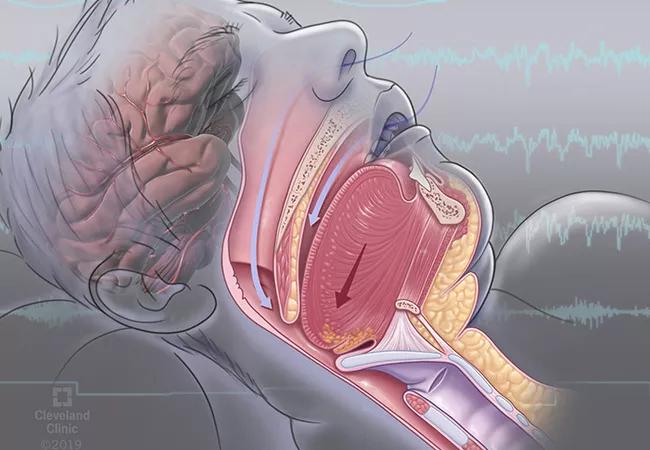
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e23945da-eaea-4263-9067-991e1c0f42dc/23-NEU-4270674-sleep-apnea-650x450-1_jpg)
23-NEU-4270674-sleep-apnea-650×450
Sleep-related hypoxia is associated with incident atrial fibrillation (AF) across three different hypoxia measurements and after adjustment for impairment of pulmonary physiology. So finds a retrospective analysis of sleep studies in more than 42,000 patients conducted at Cleveland Clinic over 15 years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our findings in a large sample implicate sleep-related hypoxia as an important biological pathway of AF and identify exposure to it as a clinically relevant driver of AF risk,” says first author Catherine Heinzinger, DO, MS, of Cleveland Clinic’s Sleep Disorders Center. “These findings are novel and clinically relevant in that prior cohort studies in this area were much smaller and their results were not definitive.”
More than 5 million people in the U.S. have AF, and studies have shown a strong association between AF and sleep-disordered breathing (SDB). Population-based studies and clinical cohorts have implicated SDB in AF development, but data on the role of sleep-related hypoxia in AF evolution and risk remain inconsistent.
“In this study, for the first time, underlying contributions of pulmonary disease to sleep-related hypoxia in the development of AF have been rigorously accounted for via consideration of objective lung function testing measures,” notes senior author Reena Mehra, MD, MS, Director of Sleep Disorders Research in Cleveland Clinic’s Neurological Institute. “Our results suggest that sleep-specific hypoxic influences are independent of decrements of underlying lung function ― and thereby provide more confidence in the notion that hypoxic mechanisms of atrial arrhythmogenesis are driven by upper airway compromise inherent to sleep-disordered breathing and not attributable to confounding by restrictive or obstructive pulmonary disease.”
“We have known for some time that patients with sleep apnea who experience significant drops in oxygen saturation during sleep are at greater risk for adverse cardiac events,” adds co-author Michael Faulx, MD, a cardiologist in Cleveland Clinic’s Section of Clinical Cardiology. “Additionally, Dr. Mehra has previously demonstrated a link between decreased oxygen saturation during sleep and increased expression of molecular markers of oxidative stress. These new findings add a clinical piece to this puzzle that further supports the importance of sleep apnea screening and treatment in patients with AF.”
Advertisement
For the new study, published in the Journal of the American Heart Association, researchers leveraged a large clinic-based registry to investigate the association between objective polysomnographic features of SDB and hypoxia relative to the longitudinal development of newly diagnosed AF. These same sleep indices also were examined in relation to AF in a smaller subset of the cohort with lung function testing data.
Adults who underwent sleep studies of at least three hours’ duration at Cleveland Clinic from 2000 through 2015 — most of whom had been referred for diagnostic evaluation for obstructive sleep apnea — were included in the study. The cohort (N = 42,057) was 51% male and 74% white. Mean age was 50.7 years, median body mass index (BMI) was 33.2 kg/m2 and 4.6% of patients developed AF within five years after their sleep study.
The presence of SDB was determined using the apnea hypopnea index (AHI). Sleep-related hypoxia was assessed using three measures of oxygen saturation (SaO2): minimum SaO2, mean SaO2 and the percentage of time that SaO2 was below 90% (T90). Sleep-related hypercapnia was evaluated using maximum end-tidal carbon dioxide (ETCO2) during the sleep study. The researchers used Cox proportional hazards models to assess associations between the above metrics and incident AF. Results were adjusted for age, sex, race, BMI, cardiopulmonary disease and risk factors, antiarrhythmic medications and positive airway pressure. In patients with available spirometry data, results were further adjusted for forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC) and FEV1/FVC.
Advertisement
The investigators found the following:
“In the full cohort, a 10-unit increment increase in AHI was associated with only a 2% increased risk for AF, and that was no longer significant after accounting for pulmonary physiology,” says Dr. Heinzinger. “On the other hand, the measures of sleep-related hypoxia had a strong association with AF risk, which was robust to pulmonary physiology.”
In participants for whom spirometry data were available, the association between T90 and AF was robust to adjustment for all three spirometry measures, with little change in the point estimate: FEV1 (HR = 1.04; 95% CI, 1.01-107), FVC (HR = 1.04; 95% CI, 1.01-1.07) and FEV1/FVC (HR = 1.05; 95% CI, 1.02-1.07).
Even though the results for ETCO2 were not statistically significant, having sufficient data to draw that conclusion is noteworthy, according to Dr. Heinzinger. ETCO2 is routinely included in sleep studies done at Cleveland Clinic, unlike most other institutions.
The authors believe their findings point to a need for a clinical paradigm shift from a focus on frequency of respiratory events to hypoxia metrics when assessing longitudinal AF risk. “A key takeaway for clinicians is that they shouldn’t assume addressing sleep apnea will always resolve hypoxia,” Dr. Heinzinger notes. “Our work sets the stage to begin identifying the endophenotype of hypoxic ventilatory instability that may be more responsive to other interventions such as supplemental oxygen.”
Advertisement
The data also have provided a foundation for future studies. Areas for exploration include novel measures with enhanced accuracy to capture specific pathophysiologic consequences of SDB and alternative lung volume measures, such as expiratory reserve volume.
“We’ve almost completed an analysis of results from 50,000 sleep studies, with the goal of computing novel metrics for sleep apnea-specific hypoxic burden, and we’ve just received a grant to study how hypoxic burden relates to AF,” Dr. Heinzinger says. “We’ll also be investigating pulse rate variability as a marker of autonomic instability and its relationship to sleep apnea.”
“The current study has yielded interesting findings,” adds study co-author Mina Chung, MD, an electrophysiologist in Cleveland Clinic’s Section of Cardiac Electrophysiology and Pacing. “Whether additional attention to residual hypoxia despite treatment of sleep-disordered breathing might reduce AF will be of interest to study.”
Advertisement
Advertisement
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
UK experts compare and contrast the latest recommendations
While results were negative for metformin, lifestyle counseling showed surprising promise
Investigational pulsed-field ablation system also yielded procedural efficiencies
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
ACC/AHA panel also upgrades catheter ablation recommendations
Retrospective analysis finds “hypoxic and sleepy” subtype to confer greatest risk
Network proximity and EHR analyses identify diabetes drug as a top candidate for risk reduction