OPTION trial demonstrates significantly less bleeding risk with comparable efficacy
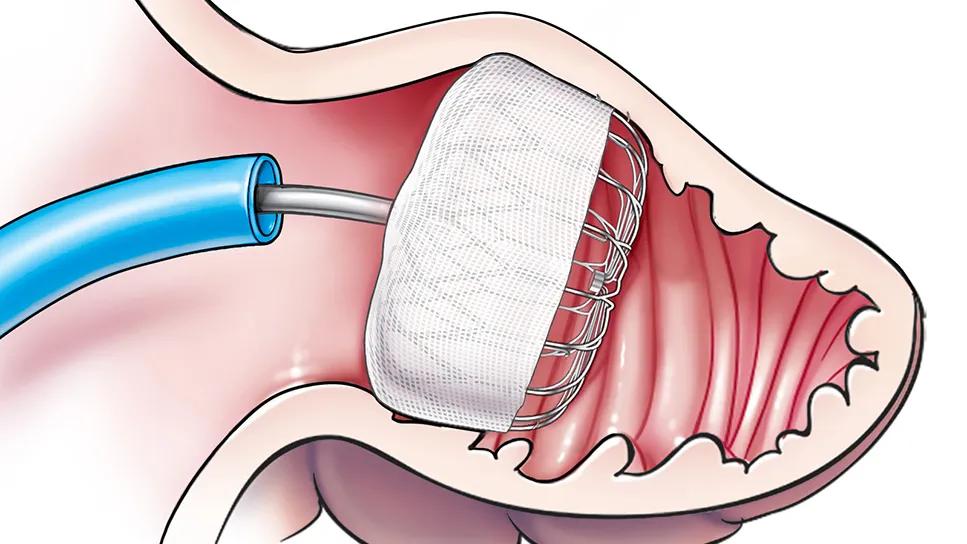
In patients at moderate to high risk of stroke who undergo catheter ablation for atrial fibrillation (AF), left atrial appendage occlusion (LAAO) significantly lowers the risk of nonprocedural bleeding compared with oral anticoagulation (OAC) while maintaining similarly low rates of stroke, death or systemic embolism.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That’s the conclusion of the first direct comparison between OAC and LAAO following AF ablation where anticoagulation therapy consisted predominantly of newer nonwarfarin direct oral anticoagulants. The findings, from the multicenter randomized OPTION trial, were presented by Oussama Wazni, MD, MBA, in a late-breaking science session at the American Heart Association Scientific Sessions 2024. They were published simultaneously in the New England Journal of Medicine.
Rates of the primary safety endpoint —nonprocedural major bleeding or clinically relevant nonprocedural bleeding through 36 months — were 8.5% with LAAO versus 18.1% with OAC. Meanwhile, rates of the primary efficacy endpoint — a composite of all-cause death, stroke or embolism — were equivalent between patients treated with LAAO (5.3%) and those receiving OAC (5.8%).
“This study has the potential to change clinical practice,” says Dr. Wazni, the study’s first author and Section Head of Electrophysiology at Cleveland Clinic. “I think patients will increasingly want to just have their left atrial appendage closed at the time of ablation and not have to worry about chronic anticoagulation, especially because the difference in bleeding rates was so large.”
While catheter ablation is well established for treating symptomatic AF, it carries a risk of AF recurrence, sometimes with minimal symptoms. As a result, guidelines endorse indefinite OAC therapy following catheter ablation in all patients at moderate to high stroke risk. However, studies have found that more than a quarter of such patients discontinue OAC therapy within a year due to the risk of OAC-related bleeding and cost concerns. Whereas studies have shown catheter-based LAAO to be a safe and effective alternative to warfarin for stroke prevention in this setting, high-quality data comparing LAAO with contemporary OAC agents are scarce.
Advertisement
“Against this backdrop,” Dr. Wazni explains, “we undertook this trial to assess whether LAAO could safely reduce bleeding risk relative to oral anticoagulation while preserving comparable protection from stroke, systemic embolism and death among patients still at risk of stroke following catheter ablation for AF.”
The OPTION investigators enrolled 1,600 patients undergoing catheter ablation for AF. Patients were from 114 global sites, and all had an elevated CHA2DS2-VASc score. Randomization was on a 1:1 basis to either LAAO or OAC following ablation.
LAAO was performed either concomitant with (40.8%) or sequentially after (59.2%) ablation. The OAC group received anticoagulation throughout the study period; 95% of these patients received a nonwarfarin anticoagulant (62% apixaban, 29% rivaroxaban, 4.6% edoxaban, 4.1% dabigatran). Choice of agent was at the treating physician’s discretion. Follow-up visits took place at three, 12, 24 and 36 months.
The primary safety endpoint of nonprocedural bleeding was assessed for superiority and included both major bleeding and clinically relevant nonmajor bleeding. The composite primary efficacy endpoint of stroke, all-cause death or systemic embolism was assessed for noninferiority.
Mean patient age was 70 ± 7.7 years; mean CHA2DS2-VASc score was 3.5 ± 1.3. “The two treatment groups were well balanced and reflected well the patient population that presents for catheter ablation,” Dr. Wazni notes.
Follow-up at 36 months was high in both groups (94% with LAAO and 93% with OAC). In the LAAO group, implant success was 99%.
Advertisement
Rates of the primary safety endpoint (8.5% with LAAO vs. 18.1% with OAC) met the criterion for superiority (hazard ratio [HR] = 0.42; 95% CI, 0.31-0.57; P < .0001 for superiority), largely driven by a difference in clinically relevant nonmajor bleeding.
Rates of the primary efficacy endpoint (5.3% with LAAO vs. 5.8% with OAC) met the criterion for noninferiority (HR = 0.91; 95% CI, 0.59-1.39; P < .0001 for noninferiority). Rates of individual components of the composite endpoint were as follows:
A secondary endpoint of major bleeding (including procedural bleeding) occurred in 3.9% of the LAAO group and 5.0% of the OAC group (P < .0001 for noninferiority, but not significant for superiority).
Prespecified subgroup analyses showed the results to be consistent when stratified by age, sex, CHA2DS2-VASc score, HAS-BLED score and type of AF.
“This trial demonstrates that LAAO can be performed safely in AF ablation patients with effective results,” Dr. Wazni observes. “The fact that the procedure can be performed at the same time as an ablation makes it a convenient and potentially appealing alternative to chronic anticoagulation therapy.”
He says the OPTION trial breaks new ground by establishing a favorable standing for LAAO relative to newer nonwarfarin anticoagulants, particularly in the post-AF ablation setting, where stroke and bleeding risks are sometimes perceived as lower. “The 18.1% rate of clinically relevant bleeding we observed in the OAC group underscores the risks inherent to long-term anticoagulant use,” he says.
Advertisement
“The OPTION trial will expand the indication for LAA closure to include patients undergoing AF ablation, along with the possibility of having these two procedures performed concomitantly in one setting,” adds study co-author Walid Saliba, MD, Medical Director of the Center for Atrial Fibrillation at Cleveland Clinic. “This makes this option very attractive and will change the way we treat patients with AF.”
“In view of these results,” Dr. Wazni concludes, “I expect that most patients who undergo catheter ablation for AF may soon likely opt for LAA closure as well.”
The OPTION trial was funded by Boston Scientific, which markets the LAAO device used in the study. Dr. Wazni reports that he has served as a consultant and speaker for Boston Scientific. Dr. Saliba reports that he has served as an advisory board member for Boston Scientific.
Advertisement
Advertisement

New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits

Large SURPASS registry study finds LAAO device safe and effective through one year

Scenarios where experience-based management nuance can matter most

Multimodal evaluations reveal more anatomic details to inform treatment

Large retrospective study suggests DOACs are safe, effective alternative to low-molecular-weight heparin in complex patient population

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve

Medical and surgical perspectives on current and emerging uses of ECMO and Impella