Analysis compares ovary removal to surveillance in asymptomatic patients
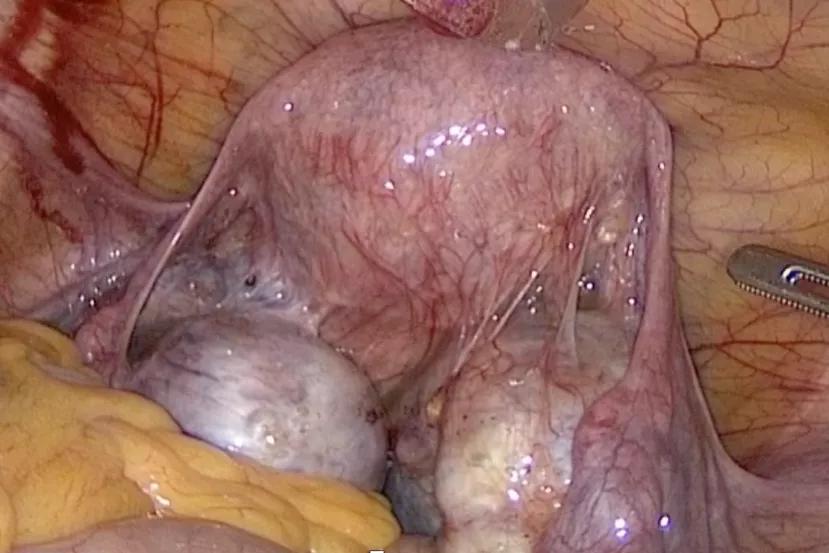
Endometriosis is associated with an increased risk for ovarian cancer. Therefore, when imaging reveals asymptomatic ovarian endometrioma in premenopausal women who are no longer interested in future fertility, gynecologists must weigh the risk of procedural complications and the potential for subsequent surgical menopause against the possibility of future ovarian pathology or cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A recent study in the American Journal of Obstetrics and Gynecology could aid clinicians and patients in their decision-making. Authored by Megan Orlando, MD, Rosanne Kho, MD and others, the study indicates that unilateral salpingo-oophorectomy is associated with improved outcomes compared to surveillance. “There is a gap in literature in terms of understanding evidence-based management of women with endometriomas as they approach menopause,” says Dr. Orlando, who recently completed a clinical fellowship in minimally invasive gynecologic surgery with Cleveland Clinic’s Ob/GYN & Women’s Health Institute. “We focused our research on asymptomatic patients because it often makes sense to remove the cyst or ovary if it’s causing pain. If there is an incidental finding in a premenopausal patient and she doesn’t want future fertility, our study shows that it would make sense to remove the whole ovary.”
Dr. Orlando and colleagues from Cleveland Clinic, Providence Saint John’s Health Center, University of Connecticut Health Center and University of Washington created a decision tree and conducted a cost-effectiveness analysis to ascertain the preferred strategy for management of incidental endometrioma: unilateral salpingo-oophorectomy (USO) or ultrasound surveillance six to 12 weeks after diagnosis, then annually.
“We calculated cost effectiveness by looking at the change in cost to achieve an effective outcome – mortality – over the change in deaths, with a willingness-to-pay threshold of $11.6 million as the value of a statistical life,” says Dr. Orlando. Using information extensively gathered from published literature, the team modeled the probabilities of surgical complications, occult malignancy, development of contralateral adnexal pathology, surgical menopause, use of hormone replacement therapy and development of ovarian cancer compared to costs incurred from surgical procedures, complications, ultrasound surveillance, hormone therapy and treatment of ovarian cancer.
Advertisement
The model demonstrated that unilateral salpingo-oophorectomy incurs fewer deaths (0.28% vs. 1.5%) and fewer cases of ovarian cancer (0.42% vs. 2.96%) with costs below the national willingness-to-pay thresholds.
“It’s important to note that we’re not saying that every patient who is premenopausal with asymptomatic endometrioma should have her ovary removed,” says Dr. Orlando. “But this is another piece of data to be used in shared decision-making with our patients.”
In addition to publishing complete results in the American Journal of Obstetrics and Gynecology, the team presented its findings at the 48th Annual Scientific Meeting of the Society of Gynecologic Surgeons in March 2022. “The gynecologist is often faced with the challenging question of the best treatment approach for patients diagnosed incidentally with an ovarian endometrioma,” says Dr. Kho. “This decision analysis model shows that the strategy of removal of the involved ovary, compared to continued surveillance, may prevent one diagnosis of ovarian cancer in every 82 patients, and one death from ovarian cancer in every 40 patients. We believe that the findings of this study contribute significantly to the literature and may guide clinicians in the counseling of patients who have been found on imaging to have an incidental ovarian endometrioma.”
Advertisement
Advertisement

Multidisciplinary teams work together in in-situ scenarios

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity