Recently launched first-of-kind study aims to address an unmet therapeutic need

Freezing of gait (FOG) eventually develops in more than half of people with Parkinson’s disease (PD). While it is generally not effectively managed with medications or surgical treatments, FOG can be ameliorated by visual gait cues such as parallel floor lines. However, the real-world applicability of such gait cues is limited. New research now underway at Cleveland Clinic is exploring whether augmented reality (AR) can help change that and expand the utility of visual gait cues to treat FOG in people with PD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
FOG is a treatment priority in PD because it is associated with falls, morbidity and mortality. While visual gait cueing has utility in reducing FOG, it requires alteration of physical spaces that is simply not feasible at scale. For instance, parallel floor lines cannot be overlaid on all the surfaces a patient with PD is likely to traverse. Other types of visual cues, like projected laser lines, have some promise but could potentially interfere with social interactions.
“There is a need for cueing techniques that are on-demand and perceptible only to the patient,” says Cleveland Clinic movement disorders neurologist James Liao, MD, PhD. “The good news is that recent advances in augmented reality are making this possible.”
Building on those advances, Dr. Liao is leading a study in which AR glasses are used to digitally project cues that are visible only to the wearer, in an effort to improve PD-related FOG. The study is receiving funding support from the American Parkinson Disease Association.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/52e79485-dba3-43e9-acb4-da4e199baa37/23-NEU-3559066-CQD-Inset-800x1120-1-731x1024_jpg)
Photo of a healthy volunteer wearing the augmented reality glasses and holding the hand control used in the study.
The study is enrolling 36 patients with PD and FOG to complete an obstacle course-like gait task under six visual cue conditions:
The AR cue is a collection of images that appear on the floor at the glasses-wearing patient’s feet and are designed to mimic laser lines projected onto the floor (see video example).
Advertisement
Video demonstrating hand-triggered visual cues as seen by a healthy volunteer wearing augmented reality glasses.
Patients’ gait is assessed both by video capture and by wireless sensors on the body that monitor the movement of each limb. The various cue conditions are used to determine whether patients improve with conventional cues, how intermittent cues perform relative to constant-on cues, and how cues triggered by an examiner perform relative to patients’ self-triggered cues.
“If successful, this will be the first investigation to show that augmented reality cues can improve freezing of gait,” Dr. Liao notes. “It could lead to widespread adoption of AR-assisted cueing devices for the treatment of freezing of gait.”
He adds that the study will also inform future AR-based gait research in PD, including whether to prioritize development of closed-loop cues (i.e., automatically triggered) or development of constant-on or patient-triggered intermittent cues.
“By comparing freezing-of-gait propensity across cue mechanisms, we may gain insight into the mechanisms of freezing of gait, which remain incompletely understood,” Dr. Liao says. “We believe this project will lead to reliable and discreet treatments for freezing of gait that can improve safety and quality of life for people with Parkinson’s disease.”
Advertisement
Advertisement

Various AR approaches affect symptom frequency and duration differently

Dopamine agonist performs in patients with early stage and advanced disease

Early assessment could affect clinical decision making

Systems genetics approach sets stage for lab testing of simvastatin and other candidate drugs

Study aims to inform an enhanced approach to exercise as medicine

New tool for general neurologists aims to streamline differential diagnosis

When and how a multidisciplinary palliative care clinic can fill unmet needs for this population
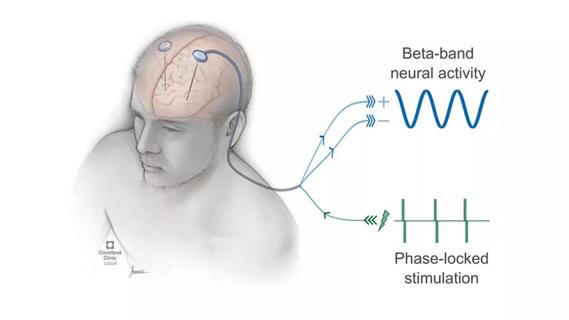
Research project will leverage insights into neural circuits to advance DBS technology