Innovations include 3 intracorporeal urinary diversion techniques
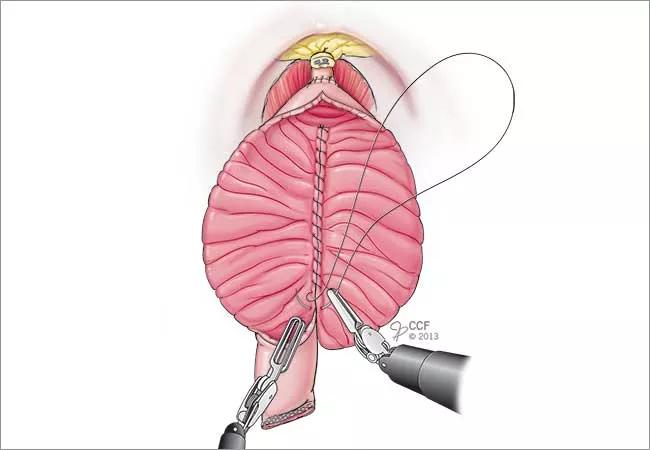
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9ef02d6f-3bba-4b79-8af7-dec7bca5ae82/650x450-Haber-Bladder-1_jpg)
650×450-Haber-Bladder
Glickman Urological & Kidney Institute urologists have performed more than 350 robotic cystectomies with intracorporeal urinary diversions, more than any other center in the United States and the second highest number in the world.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Just a few years ago, the same surgeons typically performed radical cystectomies using an open surgical approach that required a seven- to 10-day hospitalization. About 60 percent of those patients developed postsurgical complications, such as ileus, the temporary arrest of intestinal peristalsis, which causes nausea, vomiting and abdominal bloating.
Today, the team performs most radical cystectomies via a minimally invasive robotic approach, and patients are often discharged after a four- to five-day hospitalization. In addition, the urologists have gone a step further, performing many urinary diversions robotically, which allows them to avoid making another incision and exposing the bowels for this part of the procedure.
“Currently, most centers that perform radical cystectomy robotically will convert to an open approach for the urinary diversion,” explains urologist Georges-Pascal Haber, MD, PhD. “We developed a technique for robotic intracorporeal urinary diversion after bladder removal. We have used this technique to form the three major types of urinary diversion: ileal conduit, continent catheterizable pouch, and neobladder, and we found that the robotic technique has improved clinical outcomes.”
Robotic intracorporeal urinary diversions are challenging technically. But the benefits are significant and include smaller incisions, reduced postoperative pain, diminished bowel handling and exposure, and reduced risk of fluid imbalance.
“Most important,” says Byron Lee, MD, PhD, urologic oncologist and researcher, “we haven’t seen a difference in cancer control, whether we perform the cystectomy open or robotically. Additionally, there is no difference in cancer control between extracorporeal or intracorporeal urinary diversion. Many of us are now performing intracorporeal urinary diversions because of the benefit to the patient immediately after surgery.”
Advertisement
An enhanced recovery after procedures (ERAP) program covering pre-, intra- and postoperative periods has improved postoperative outcome metrics as well. The program addresses a number of factors that enhance patient recovery after surgery. Some of the essential elements include intense perioperative patient education, avoiding fasting and bowel prep which can deplete the body of vital fluids and nutrition immediately before surgery, avoiding nasogastric tube placement, minimizing opioid use, and encouraging early ambulation in the recovery phase. The program has reduced overall length of stay by 29 percent, postsurgery emergency department visits by 40 percent, readmissions by 39 percent, and costs by 14 percent.
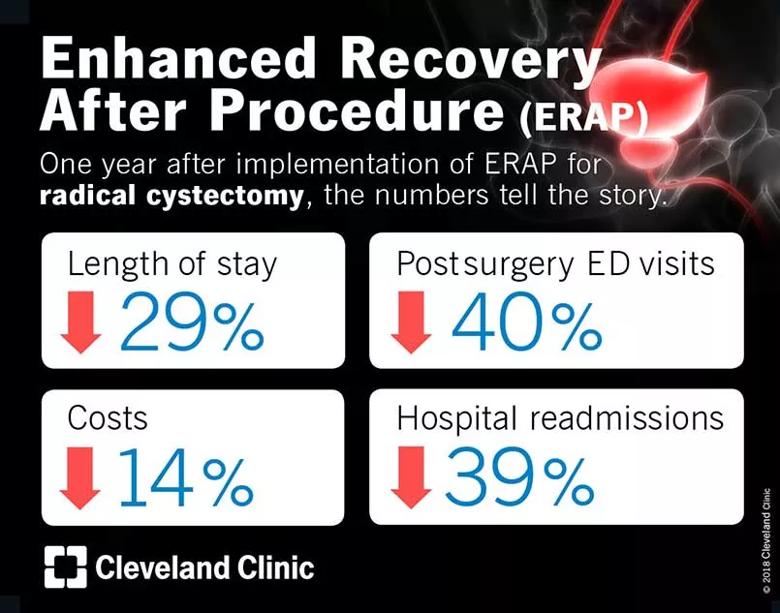
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d113075-d31c-46be-90bb-6e5b5bd8c8e2/805x-ERAP_jpg)
Drs. Lee and Haber also are exploring a form of distance health to lower complication rates. Dehydration is a problem that can land radical cystectomy patients back in the hospital if fluid intake is inadequate after discharge.
“It could be that the patient’s bowels aren’t functioning perfectly after surgery, so their appetite is not the best,” says Dr. Lee. “But we do not have a good way to monitor intake post-discharge. Readmission due to dehydration is hard on the patient, and of course costly.”
He and Dr. Haber are experimenting with giving patients “smart bottles” that can record a patient’s fluid intake and send the data to a cloud server where doctors can access and assess it.
“We are always looking for opportunities to improve care that could result in better outcomes,” says Dr. Haber.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key