Weighing considerations among microvascular decompression, rhizotomy and more
A myriad of surgical options are available for patients with trigeminal neuralgia (TN) who are not helped by medications, and choosing the one that’s most likely to offer pain relief requires thorough clinical and radiological assessment. So emphasized neurosurgeon Varun Kshettry, MD, at a recent Cleveland Clinic virtual symposium on TN management available online as 10 video presentations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“One of the leading causes of unsuccessful surgery for trigeminal neuralgia is failed decision-making in patient selection,” says Dr. Kshettry, Surgical Director of Cleveland Clinic’s Trigeminal Neuralgia Program. “At Cleveland Clinic, we are fortunate to have all headache and facial pain-related specialties at the same location within our Neurological Institute, facilitating the necessary consultation among medical and surgical experts.”
Considerations around patient selection for surgical interventions for TN were covered in symposium talks by Dr. Kshettry and Gene Barnett, MD, MBA, Director of Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center and a neurosurgeon with its Gamma Knife Center. Highlights are recapped below. (See the companion Consult QD post here for an overview of nonsurgical treatment options in the context of optimal multidisciplinary TN management.)
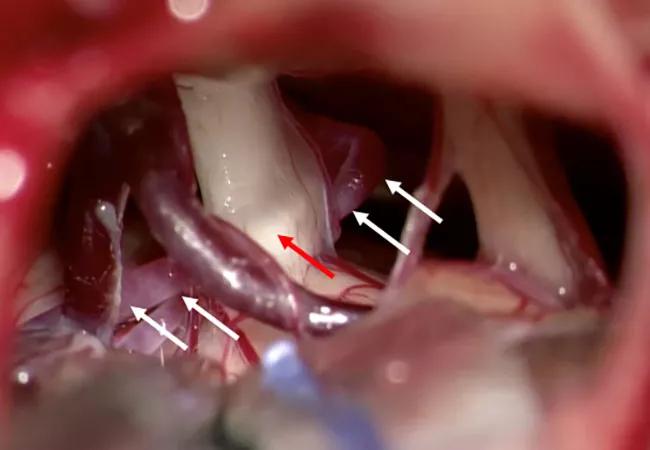
For patients with vascular compression of the trigeminal nerve and classic TN symptoms, microvascular decompression surgery (MVD) treats the problem with low risk of nerve injury and offers the best chance of long-term relief. However, MVD should be offered only to patients deemed likely to benefit. The surgery requires a small craniotomy to mobilize the compressing blood vessel off the impacted trigeminal nerve, and frequently Teflon™ padding is used to keep them separated (see Figure).
Dr. Kshettry, who specializes in MVD for TN, considers the following in assessing candidacy for the procedure:
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a1461564-c8ec-498a-9235-6c00873a36a2/22-NEU-2635112-CQD-Inset-800x570-1_jpg)
Figure. (Top left) High-resolution MRI demonstrating an artery (red circle) compressing the trigeminal nerve (yellow). (Top right) Initial intraoperative view of right-sided microvascular decompression demonstrating loop of an artery (white arrows) causing severe compression and denting (red arrow) of the trigeminal nerve. (Bottom left) View after the arterial loop was dissected free of attachments and mobilized and transposed away from the nerve to the tentorium. (Bottom right) View after Teflon™ was used to secure the arterial loop to the tentorial membrane. No vessel or even Teflon is touching the nerve at the end of the procedure. Note: Normal petrosal veins (asterisks) are preserved, as they are not touching the nerve.
Rhizotomy may be used to treat TN in patients for whom medical management is inadequate, especially if they are unsuitable for MVD, including individuals with multiple sclerosis and those without vascular compression.
The major types of rhizotomy are outlined below. All induce pain relief by directed strategic injury to the trigeminal nerve, so they may result in permanent side effects such as facial numbness.
Radiofrequency rhizotomy is the oldest method. While it offers good results, it requires mapping by triggering pain episodes on an awake patient. As this pain can be excruciating intraoperatively and good alternatives are available, this procedure has become less common. It also has the highest risk of anesthesia dolorosa — a gnawing, aching pain that is very difficult to treat.
Advertisement
Glycerol rhizotomy offers rapid pain relief with low risk of long-term numbness. However, recurrence is common and there is risk to other nerves in the head.
Balloon compression rhizotomy is targeted to the Gasserian ganglion. Initial pain relief is high, and side effects and complications are low. It often yields relief that lasts for years.
Radiosurgery (Gamma Knife®) rhizotomy is aimed at the trigeminal root in the posterior fossa. It typically takes about a month to obtain pain relief. Although fewer than half of patients achieve complete pain relief, the majority have good relief by 12 months.
“All four rhizotomy methods can produce reasonable duration of relief with acceptable side effects, and I have used them all during my career,” says Dr. Barnett. “However, I have exclusively used balloon compression and Gamma Knife rhizotomy for the past 20 years.”
Separating the trigeminal nerve fascicles into six to eight bundles is a newer procedure for patients with classic TN without vascular compression. Although almost all patients report facial numbness postoperatively, many at least partially recover within six months. While early data suggest that this may yield similar degrees of pain relief as patients who have vascular compression, larger patient series and longer follow-up studies are needed to adequately assess safety and efficacy, Dr. Kshettry notes.
“Many factors must be considered when determining the best treatment option for trigeminal neuralgia, including the likelihood of whether a procedure will be successful for a given patient, the need for rapid relief and what potential side effects may be tolerated,” Dr. Kshettry concludes. “Collaboration with colleagues and a frank discussion with the patient are essential to optimizing outcomes for this highly complex syndrome.”
Advertisement
Advertisement

Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains