Study of over 5,000 patients shows type of surgery matters too
By Bradley C. Gill, MD, MS; and Navin Sabharwal, BS
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Benign prostate enlargement (BPH), also known as benign prostate hypertrophy or hyperplasia, is a common condition in aging men. It most often presents with lower urinary tract symptoms, including a weak or dribbling urinary stream, a feeling of incomplete bladder emptying after urinating, frequent trips to the bathroom (frequency), and a bothersome sudden and severe urge to urinate (urgency).
Physicians first attempt treating BPH with medications that either relax muscle within the prostate over a couple days (alpha adrenergic blockers) or shrink the prostate gland over a few months (5-alpha reductase inhibitors). Additionally, some men are prescribed medications to help calm the bladder and reduce the symptoms of urgency and frequency (anticholinergics or beta-3 agonists).
While many men do well with medical therapy for BPH, some do not tolerate medications due to side effects. Likewise, many men prefer to avoid a lifetime of daily medication with its ongoing costs and the hassle of refilling a prescription.
These drawbacks led members of Cleveland Clinic Glickman Urological & Kidney Institute’s Mens’ Health team to investigate how effective surgical procedures for BPH are at enabling men to discontinue their urologic medications. All BPH surgeries performed in the Cleveland Clinic health system from 2001 to 2016 were analyzed – some 5,150 procedures.
The focus of the study was to determine whether tissue-eliminating procedures achieved better rates of medication discontinuation compared to tissue-necrosing procedures.
Advertisement
Tissue-eliminating procedures included transurethral resection of the prostate (TURP), laser photovaporization of the prostate and simple prostatectomy. Tissue-necrosing procedures included transurethral microwave therapy or transurethral needle-ablation, which were grouped in analyses.
Men included in the study were an average 69 to 72 years of age with variable rates of medication use before surgery:
As expected, data showed that men who underwent surgeries that eliminated prostate tissue were more likely to avoid BPH medications than men who underwent surgeries that damage prostate cells to subsequently shrink the gland through necrosis or cell death.
Specifically, looking at medication use beyond 12 months from surgery, tissue-eliminating procedures achieved significantly better rates of medication discontinuation compared to tissue-necrosing procedures, respectively:
Similarly, men who were not on a specific type of medication at baseline were significantly less likely to initiate these medications if they had undergone a tissue-eliminating versus tissue-necrosing procedure:
Advertisement
Taken together, the results of the study show that surgical procedures eliminating prostate tissue were associated with higher rates of medication discontinuation than procedures that shrink the prostate gland by inducing tissue necrosis. Similar findings were noted for men and medication initiation.
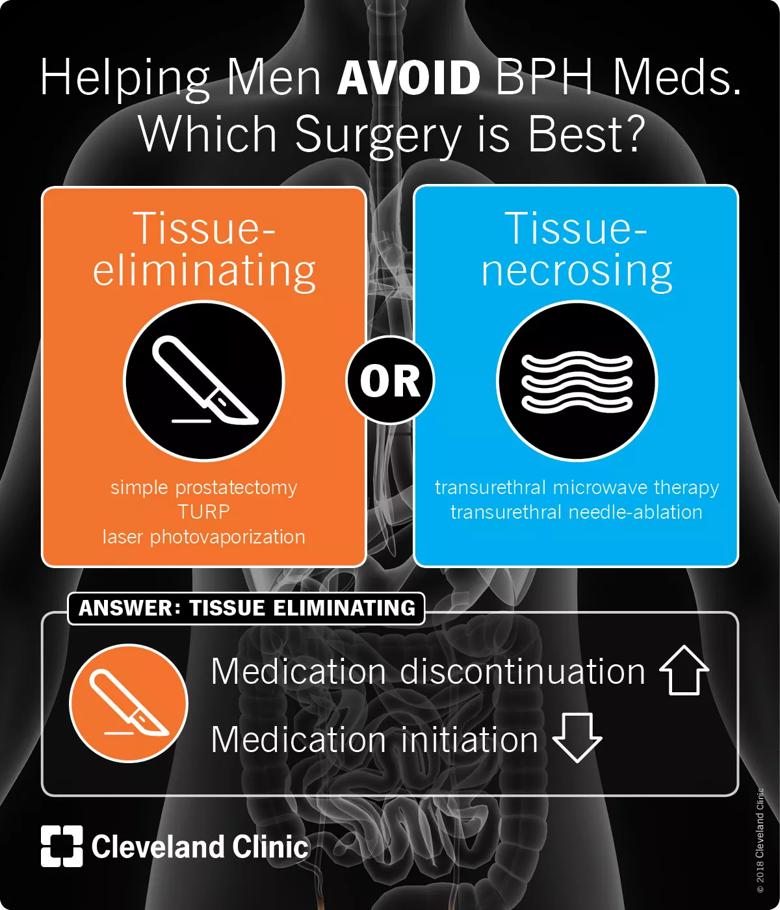
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/143d6833-0647-47a9-af3a-c682faff858a/18-URL-758-Visual-Abstract-BPH-Surgery_jpg)
In all, it appears surgical procedures for BPH help men avoid urologic medications. Those that eliminate tissue fared better than those that shrink the prostate by causing necrosis, likely because they achieve a greater decrease in prostate size and reduction of the tissue obstructing urinary flow.
In this series, simple prostatectomy performed best, followed by transurethral prostate resection and laser photovaporization, with the tissue-necrosing procedures outperformed by all of these.
Which procedure a man pursues for his BPH, however, is based upon a number of clinical factors and an informed discussion with his surgeon.
Mr. Sabharwal is a medical student at Lerner College of Medicine and Dr. Gill is a Chief Resident in the Department of Urology. Urologists Daniel Shoskes, MD; James Ulchaker, MD; and Khaled Fareed, MD, also participated in this study.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key