Phase 1b trial shows good response rate
Despite improvements in surgery, radiation and chemotherapy, 40,000 women still die each year from breast cancer, many from its most aggressive form, HER2+ breast cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Results of a phase 1b study demonstrate that a new drug combination offers a promising regimen to attack HER2, a protein that promotes the growth of cancer cells.
“About 25 percent of breast cancers are HER2+, and they tend to be more aggressive,” says Jame Abraham, MD, Director of the Breast Medical Oncology Program at Cleveland Clinic Cancer Center. “Fortunately, in the past 10 to 15 years, we have developed several new treatment options for HER2+ breast cancer that specifically target the HER2 protein. One is trastuzumab emtansine, T-DM1. Unfortunately, not all patients respond to it.”
Dr. Abraham is the principal investigator of a multi-institutional phase 1b clinical trial sponsored by the National Surgical Adjuvant Breast and Bowel Project (NSABP). The trial, called NSABP FB-10, combines T-DM1 and neratinib to treat women with metastatic HER2+ breast cancer who relapsed or progressed after trastuzumab– and pertuzumab-containing regimens. Dr. Abraham recently presented data from the trial at the 2018 American Society of Clinical Oncology annual meeting.
“Neratinib was recently approved for treatment in early HER2+ breast cancer but not metastatic breast cancer,” he says. “This particular trial is testing this drug in combination with T-DM1 in women who have HER2+ metastatic breast cancer.”
In the trial, patients received concurrent therapy with T-DM1 (3.6 mg/kg IV) on day 1 of a 21-day cycle and neratinib as a continuous daily oral dose. The neratinib dose-escalation included four dose levels — 120 mg, 160 mg, 200 mg and 240 mg — and used a 3+3 design.
Advertisement
Twenty-four patients were evaluable for toxicity, and 20 were evaluable for efficacy. Dose-limiting toxicity occurred in six patients during cycle one. Treatment-related grade 3 toxicities included diarrhea (five patients), thrombocytopenia (four patients) and ALT elevation (one patient).
The duration of the response lasted from 42 days to over 600 days. There was not a correlation of dose and peak or steady-state levels; responses were seen at all doses.
Overall the combination of full-dose T-DM1 and neratinib at 160 mg/d was well tolerated. The overall response rate was 64 percent, with four patients experiencing a complete response (CR) and nine experiencing a partial response (PR). (Updated data from the 2018 San Antonio Breast Cancer Symposium show a 63 percent response, with three patients experiencing CR and nine PR.)
“That’s actually pretty high, and we’re really happy with that,” Dr. Abraham says. “We have some patients going on almost two years on this regimen.”
A phase 2 trial to further test the safety and effectiveness of the drug combination is already started. Depending on the results, Dr. Abraham says, a phase 3 trial may compare patients treated with T-DM1 versus those treated with T-DM1 and neratinib.
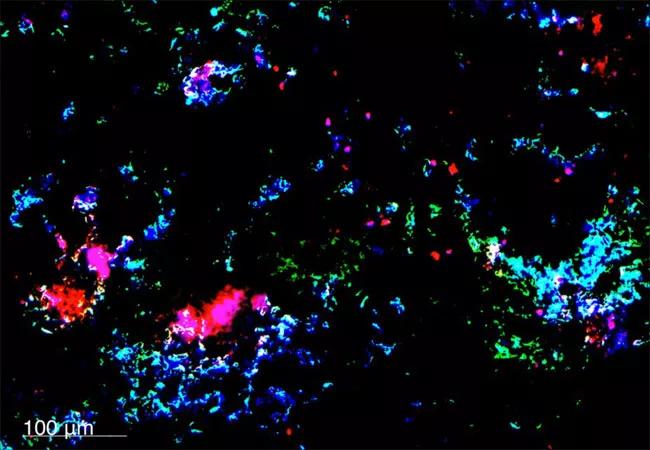
Image: Nanoparticles in breast cancer metastases. Image source: National Cancer Institute/Case Western Reserve University
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors