But the combination increases toxicity risks
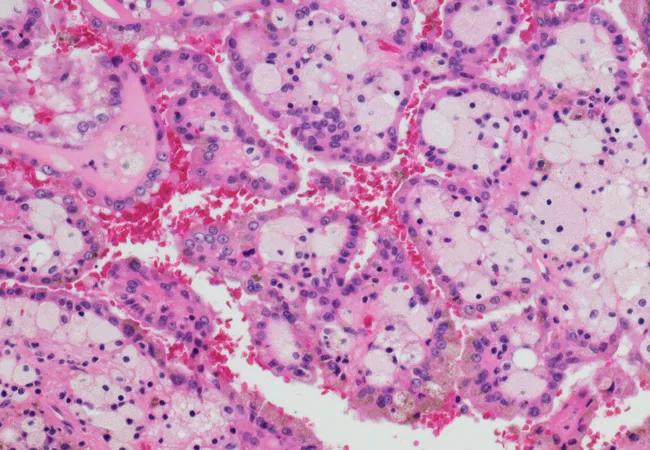
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/85c53d0a-5325-44c8-90cc-cd7950ed5c10/microRCC_650x450_jpg)
microRCC_650x450
Clinical trials have shown that targeted therapies, including tyrosine kinase inhibitors (TKIs) and mTOR inhibitors, increase survival rates for patients with metastatic renal cell carcinoma (RCC) by a significant 9 months. Those studies, however, did not include patients with RCC brain metastases, which occurs in about 10 percent of patients with metastatic RCC.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With this in mind, Cleveland Clinic physicians recently conducted a retrospective study to find out if targeted therapies would offer the same benefit to patients with RCC brain metastases. They also explored whether using targeted therapies along with stereotactic radiosurgery (SRS) — the gold standard for treating patients with limited brain metastases — offers better local brain control for patients with RCC brain metastases and whether this combination increased the risk of toxicity (namely radiation necrosis [RN]).
“The reason we wanted to do our study was the patients in those clinical trials did not have brain metastases, and that left us with some questions,” says Aditya Juloori, MD, third-year resident, radiation oncology, Cleveland Clinic Cancer Center who presented the research at the 2017 ASTRO Annual Meeting. ”For instance, is the prognosis so poor for patients with RCC brain metastases that there’s no benefit at all to giving drugs we know work well in metastatic RCC without brain involvement?”
Dr. Juloori and colleagues examined records from 1998-2015 of 376 Cleveland Clinic patients with RCC brain metastases. They found a total of 376 patients with 912 lesions. It’s the largest group that’s been studied to evaluate the use of targeted therapies for patients with RCC brain metastases.
They looked at overall survival (OS), cumulative incidences of local failure (LF), distant intracranial failure (DIF) and RN. They also recorded and analyzed timing of targeted therapies, TKIs and mTOR inhibitors.
Advertisement
Dr. Juloori and colleagues found OS was 9.7 months, similar to the benefit that targeted therapies give to metastatic RCC patients without brain metastases. They also found targeted therapies do not increase the rate of local control when used with SRS. “We know SRS works well,” Dr. Juloori says. “This suggest that whatever impact it is doing to increase survival has nothing to do with brain control.”
Finally, they found that the patients who received targeted therapies within 30 days of SRS had an 11 percent chance of developing RN versus 6 percent for those who only receive SRS. RN can cause headaches, nausea, vomiting, weakness and numbness. It can often be treated with steroids, but such drugs have their own side effects.
Dr. Juloori says that prospective studies are needed to determine the optimal timing of targeted therapies with SRS. “The challenge moving forward is trying to figure out the best timing,” he says. “It’s hard to not give a drug that improves survival, but we now know it may be best to not give it with 30 days of SRS. So what is the right time, five days later, 10? Can we pick it up later and not lose the survival benefit?”
Dr. Juloori says researchers are studying a range of cancers and targeted therapies to figure out these kinds of tradeoffs for patients with lung cancer and melanoma as well. They want to know the balance between the benefits targeted therapies provide and the potential toxicity.
“We know that targeted therapies are an integral part of the treatment for patients with metastatic renal cell carcinoma, and we know that stereotactic radiosurgery is an important part of the management of patients with brain metastases,” he says. “Now we want to find a way to make them as safe as possible so our patients not only live longer but have good quality of life while they do.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting