Improvements enable targeting of brain tumors with single-session, fractionated or neoadjuvant approaches
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2241774/14278650)
Since the inception of Gamma Knife® technology more than 55 years ago, this stereotactic radiosurgery platform designed to treat brain tumors has never stopped evolving.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
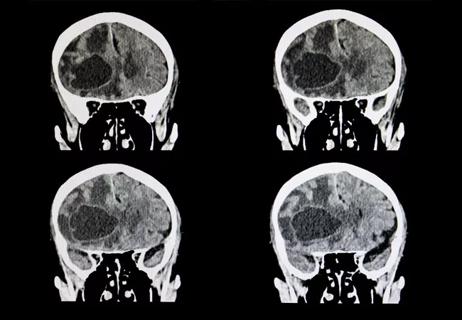
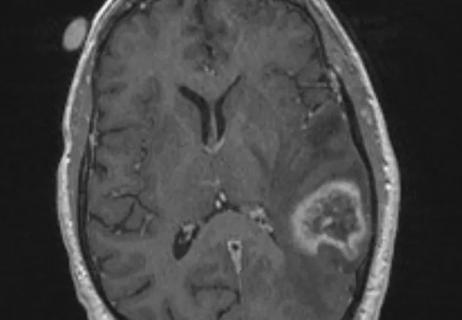
“In its current iteration, Gamma Knife uses 192 beams of radiation, all focused on a single point,” says Samuel Chao, MD, Associate Director of the Gamma Knife Center at Cleveland Clinic. “We aim to direct these beams to the tumor and cover the entire tumor with focused, high-intensity radiation while sparing the surrounding brain tissue as best as we can.”
In the latest episode of Cleveland Clinic’s Cancer Advances podcast, Dr. Chao talks about advances in Gamma Knife radiosurgery. He delves into:
Click the podcast player above to listen to the 20-minute episode now, or read on for a short edited excerpt. Check out more Cancer Advances episodes at clevelandclinic.org/podcasts/cancer-advances or wherever you get your podcasts.
Podcast host Dale Shepard, MD, PhD: It’s hard to count the number of times one goes on hospital service and someone comes in with a brain metastasis, after which both radiation oncology and neurosurgery are consulted. What are the respective types of situations where radiation is clearly better and where surgery is clearly better?
Dr. Chao: Oftentimes we think about radiosurgery as our No. 1 modality for treating brain metastases because it’s noninvasive and it’s really easy to do. It gets patients back on their feet faster. They can go on to systemic therapies much more quickly than if we do something invasive like a craniotomy. That being said, craniotomy to take out tumor still has its role in terms of the management of brain metastases.
Advertisement
Surgery may be beneficial for patients who are very symptomatic and for tumors that are extremely large — impinging heavily on the brain and causing a lot of swelling in the surrounding brain tissue. So when we go and see a patient on the hospital floor together with neurosurgery, that allows us to chat and decide on what’s the best option for the patient.
One thing we have started doing over the past several years is to even consider doing Gamma Knife radiosurgery before doing surgery — what we call neoadjuvant radiosurgery. This can make things a lot more straightforward and make treatment happen a lot more quickly. The neurosurgeons don’t have to wait for us to do radiation to clean up the resection cavity. This approach makes the radiation much tighter. It prevents development of leptomeningeal disease and reduces the risk of radiation necrosis. For many of the patients in the scenario you describe, even those in whom we decide we want to do surgery, sometimes we can strategize by doing some radiosurgery in advance to essentially “sterilize” the tumor.
Advertisement
Advertisement

Largest study to date comparing direct-acting oral anticoagulants to low-molecular-weight heparin

Research demonstrates improved overall survival for patients receiving comprehensive treatment for breast cancer in addition to radiation or surgical intervention for brain cancer
This approach led to local control for patients with brain metastases more than 2 cm in diameter
We now have an expanded toolbox to extend survival and lessen treatment toxicity

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Large retrospective study suggests DOACs are safe, effective alternative to low-molecular-weight heparin in complex patient population

Advances in genomics, spinal fluid analysis, wearable-based patient monitoring and more

An update on the technology from the busiest Gamma Knife center in the Americas