Finding variants of uncertain significance does not increase the rate of contralateral prophylactic mastectomies

Testing for the BRCA1 and BRCA2 genes has been routine for women diagnosed with breast cancer who have risk factors for hereditary breast or ovarian cancer. In consultation with genetic counselors and physicians, positive results for BRCA1/2 inform a woman’s treatment decisions. Women with positive genetic test results who choose to undergo contralateral prophylactic mastectomy (CPM) may reduce their risk of dying from breast cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many additional genes have been found to be associated with an increased risk of breast cancer, and in the past several years, multigene panel testing (MPT) has become common for this population. MPT can provide women who are diagnosed with breast cancer valuable knowledge about their hereditary risk. However, patients may be confused by the implications of positive results to variants of low or moderate penetrance. Findings that show variants of uncertain significance (VUS), which are mutations that have an unknown effect on protein function, may also confuse patients. Recent research at Cleveland Clinic sought to address concerns that positive results from MPT might cause women to choose CPM even when their overall risk profile does not indicate a strong necessity for such treatment.
“We investigated the hypothesis that multigene panel testing in patients with triple negative breast cancer (TNBC) does not result in an inappropriately high rate of bilateral mastectomy when patients are provided pre- and post-test genetic counseling,” says lead researcher Holly Pederson, MD, Director of Medical Breast Services at Cleveland Clinic’s Breast Center. Dr. Pederson presented the results of the study at the Southern Surgical Association Conference on December 5.
Dr. Pederson and her team conducted a retrospective electronic medical records-based study of women who were treated for triple negative breast cancer at Cleveland Clinic and who underwent MPT between Sept. 2013 and Feb. 2017. “We chose to investigate patients with TNBC since the majority of these patients qualify for genetic counseling, and their surgical choices are not as likely to be influenced by tumor-biology-related factors,” says Dr. Pederson.
Advertisement
The study identified 331 patients with TNBC who met the criteria for genetic counseling, and 226 opted for genetic testing (MPT – 130, BRCA1/2 – 96). All of the patients received genetic counseling before the tests, and patients with significant results were also counseled afterward. Results were as follows:
The decision to undergo CPM did not differ significantly between VUS+ and Mut- (P = 0.368) patients, within different age groups (< 40, 40-60 and > 60 years). Within the VUS+ group, Caucasians were more likely to choose CPM than other races (25.8 percent vs 9.1 percent), although this difference did not reach statistical significance (P = 0.162).
In five patients, MPT showed non-breast cancer related genetic alterations that were clinically actionable. Following is a summary of those findings:
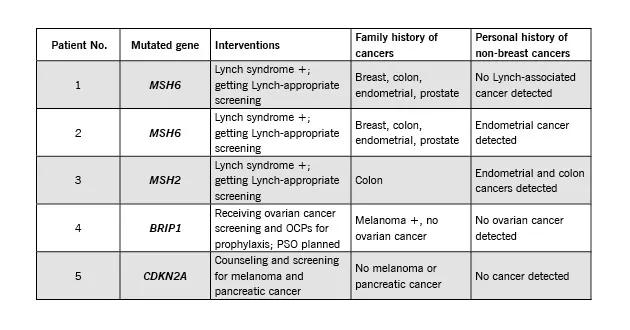
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ad09c19d-3eca-4c0f-969b-23772abc85f9/summary-chart_630x330_jpg)
“We are seeing a shifting paradigm away from single syndrome testing and towards next generation sequencing of multiple genes in clinical cancer genetics,” says Dr. Pederson. “This is particularly important for patients with triple negative breast cancer as mutations are not uncommon and can inform surgical decision making.”
The study found that with appropriate genetic counseling, detection of VUS — which are more common in gene panels — did not lead to excessive rates of CPM.
Advertisement
Dr. Pederson adds that in this study, MPT allowed for the identification of other gene mutations that supported management of the patients and their family members.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists