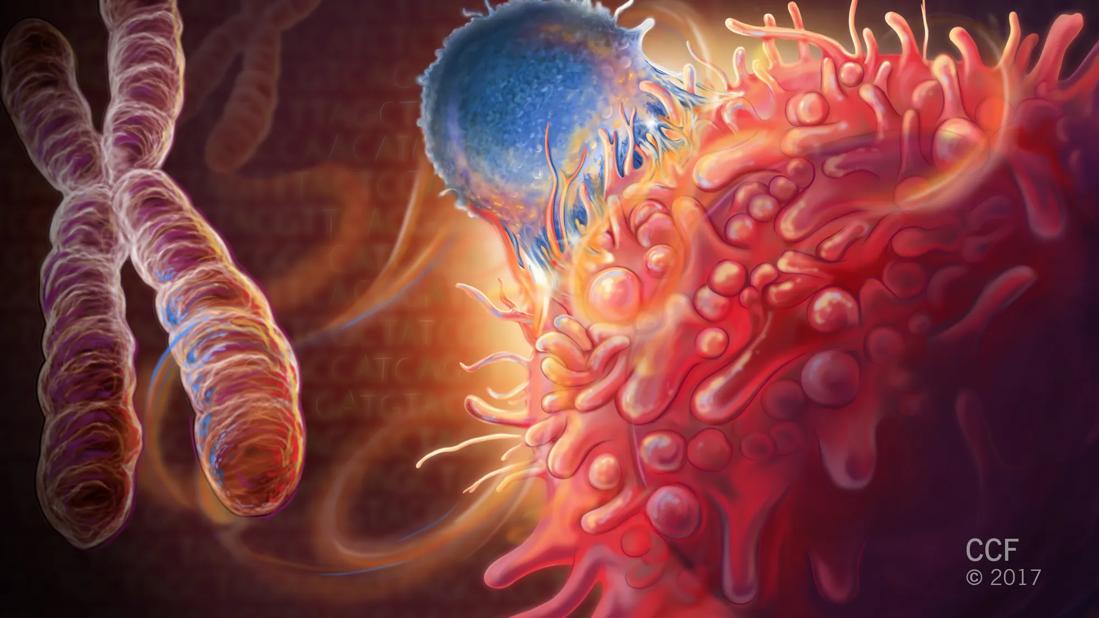
Study explores atezolizumab for myelodysplastic syndrome
Aside from lenalidomide for a small subset of patients, there’s really only one class of FDA-approved medications for patients with myelodysplastic syndrome (MDS), hypomethylating agents (HMA).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“That’s not a lot for a disease that affects between 60,000 and 170,000 people in the U.S.,” says Aaron Gerds, MD, MS, of Cleveland Clinic Cancer Center.
While HMAs — namely azacitidine and decitabine — are effective for many, there are limited treatment options (outside of bone marrow transplant) for MDS patients who don’t respond to them. That, combined with research showing higher PD-L1 expression in MDS patients who fail HMA therapy, has triggered multiple studies on the role of immunotherapy in MDS.
Three of them, including a study by Dr. Gerds, were presented in tandem at the 2018 American Society of Hematology meeting in San Diego.
“It’s tough to interpret these studies because they’re only phase 1 and 2, and survival outcomes take years to track,” says Dr. Gerds. “But immunotherapy has been so successful in lymphoma, lung and other cancers that it makes sense we start exploring it for myeloid hematologic malignancies too.”
Dr. Gerds and a multicenter team researched the safety and tolerability of anti-PD-L1 monoclonal antibody atezolizumab, both with and without HMA azacitidine, in MDS patients who had either failed or never received conventional HMA therapy.
More than 40 MDS patients (median age 76) made up three cohorts:
Advertisement
Overall response was 0 percent for Cohort A (with median overall survival of 5.9 months), 9 percent for Cohort B (with median overall survival of 10.7 months) and 62 percent for Cohort C (with median overall survival undetermined as eight patients remain on therapy).
However, the study was terminated early because of adverse events, including death.
More than 30 percent of patients receiving the combined therapy (Cohorts B and C) had grade 3-5 febrile neutropenia (compared to 10 percent of those receiving the monotherapy, Cohort A).
Serious adverse events caused all six deaths (29 percent of patients) in previously untreated patients (Cohort C). Deaths in cohorts A (70 percent of patients) and B (64 percent of patients) were more commonly due to disease progression. Nearly 30 percent of deaths in Cohort C occurred within 90 days of the study treatment, compared to a median of 160 days in Cohort A and 299 days in Cohort B.
“We had expected Cohort C — the patients who hadn’t had prior treatment — to be the healthiest and fittest, not the one with the most unfavorable safety profile,” says Dr. Gerds. “Our study reinforces that patients with MDS can be frail, and new combinations of drugs can cause unexpected toxicities. It’s a word of caution to the medical community.”
Moving the field forward and finding better treatments for patients is a must, he notes. But physician researchers should proceed cautiously and methodically. More needs to be understood about the toxicity differences between MDS patients who have failed HMA treatment and those that never received it. That will inform future studies combining HMA and immunotherapy.
Advertisement
“Immunotherapies have done a lot of good for many cancer patients. That’s why studies like ours need to be done,” says Dr. Gerds. “But we should start by dipping a toe in the water, not jumping in with both feet. First, do no harm.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient