In the U.S., fewer COVID-19 related deaths on weekends

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/25f17d85-07ed-4890-8862-ee13aaf6d10b/650x450-COVID_jpg)
650×450-COVID
By Hany Aly, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It is true that not all patients with COVID-19 need hospitalization, however, patients whose clinical presentation warrants physician management will require hospital admission. In healthcare, the pervasive phenomenon known as the ‘weekend effect’ suggests that patients admitted to hospitals on Saturday and Sunday have an increased risk of death.1 Although this is a controversial area, the majority opinion is that the weekend effect is deleterious to patient care. While the cause of this effect is unclear, the weekend effect on mortality is apparent across a range of disease presentations.1
A 2017 meta-analyses of 97 studies showed that patients admitted on the weekends had a significantly higher overall mortality (relative risk, 1.19; 95% confidence interval, 1.14-1.23).2 With regard to subgroup analyses, patients admitted on the weekends consistently had higher mortality than those admitted during the week, regardless of the levels of weekend/weekday differences in staffing, procedure rates and delays, and illness severity.2 Contradictory studies such as that by Freemantle et al, showed that the likelihood of death by all causes is less on a weekend day than on a mid-week day.3 Research continues on this matter to better understand the reasons and implications of the weekend effect and how caregivers may address them.
To determine the extent to which the weekend effect is associated with COVID-19 mortalities, we recently surveyed COVID-19 deaths within the U.S. using data presented by the Worldometer.4 We specifically assessed the difference between deaths that occurred Monday-Friday (weekdays) versus those that occurred on Saturday and Sunday (weekend) from March through October. Examination of COVID-19 associated deaths in the U.S. showed significantly fewer deaths on Saturday and Sunday, compared to deaths on weekdays (Z = 3.52673, p = 0.00042) (Figure 1). While we weren’t able to determine factors such as illness severity at time of admission and staffing level differences during the week versus on the weekend, this is still an interesting finding and something that should be investigated further. Interestingly, the “weekend effect” we report for COVID-19 in the U.S. does not exist in other countries such Germany, Italy, Iran and Turkey.
Advertisement
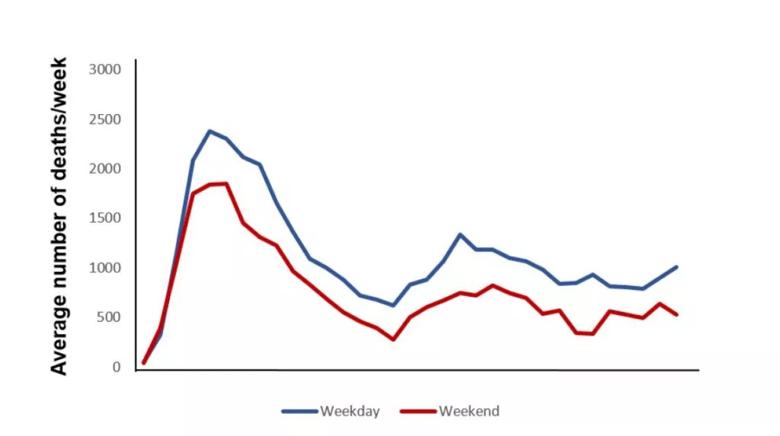
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/90df21c5-d697-4916-b1a1-07563f1acf84/fig1-1024x573_jpg)
Figure 1. Average weekday and weekend deaths associated with COVID-19 in the U.S.(2)
During a global pandemic, such as what we are experiencing with COVID-19, taking a closer look at mortality rates and understanding the reasons for fluctuations allows caregivers to assess their practices to provide the best outcomes for patients. Further studies, with detailed clinical data are urgently needed to investigate the drivers of and causes for the risk of death on weekdays/weekends from COVID-19.
Advertisement
Advertisement
Patients report improved sense of smell and taste
Clinicians who are accustomed to uncertainty can do well by patients
Unique skin changes can occur after infection or vaccine
Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition
As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients
Early results suggest positive outcomes from COVID-19 PrEP treatment
Could the virus have caused the condition or triggered previously undiagnosed disease?
Five categories of cutaneous abnormalities are associated with COVID-19