Study shows risk of overtreating patients
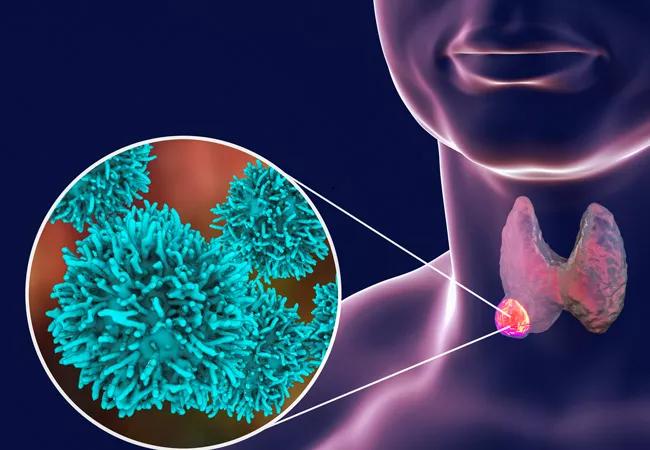
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7c6ac99e-807c-4f73-bf05-a3f6d78f9162/thyroid-cancer-650x450_jpg)
thyroid-cancer-650×450
Previous studies have shown that patients with well-differentiated thyroid cancer (WDTC) who are treated with resection followed by radioactive iodine (RAI) have a small but significant risk of developing leukemia.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Now a new study by Cleveland Clinic researchers shows that such patients have an early and significantly increased risk of developing two types of leukemia, acute myeloid leukemia (AML) and chronic myeloid leukemia (CML). The study also shows that patients who develop AML as a second cancer have worse survival.
“Several studies in the past have looked at the risk of developing leukemia in well-differentiated thyroid cancer patients who receive surgery followed by radioactive iodine, but they grouped together all different kinds of leukemias under one broad category,” says Sudipto Mukherjee, MD, MPH, associate staff in the Department of Hematology and Oncology and senior author on the study, published recently in the Journal of Oncology.
“Analyzing all leukemia subtypes under one category may not reflect true risk,” he says, “because not all leukemia subtypes behave the same way, are treated the same way or have the same prognosis.”
Dr. Mukherjee and his colleagues did a retrospective analysis of patient data from 1973 to 2016, using the Surveillance, Epidemiology, and End Results Program (SEER) registries of the National Cancer Institute, to identify the risk of development of several types of hematologic malignancies in WDTC patients treated with RAI.
The investigators analyzed 148,215 patients diagnosed with WDTC of which 53 percent received surgery alone and 47 percent received surgery followed by RAI. After a median interval of 6.5 years, 783 patients developed hematologic malignancies — 417 after surgery alone and 366 after surgery plus RAI.
Advertisement
The researchers then analyzed the risk of developing seven types of hematologic malignancies. In addition to AML and CML, they also looked at acute lymphoblastic leukemia, chronic lymphocytic leukemia, Hodgkin lymphoma, non- Hodgkin lymphoma and multiple myeloma. The elevation in risk following RAI exposure was significant only for AML and CML.
Dr. Mukherjee and his co-authors also found that the patients who developed AML and CML did so quickly — within one or two years of receiving surgery and RAI. RAI was associated with decreased leukemia-free survival for AML and CML in these patients.
Additionally, the investigators found that the patients with WDTC who developed AML after surgery and RAI did not survive as long compared with patients with WDTC who did not develop AML (median of eight vs 31 years).
“If you develop AML as a first cancer versus as a second cancer after having well-differentiated thyroid cancer treated with surgery and radioactive iodine, survival is adversely affected,” says Dr. Mukherjee. “AML occurring after RAI behaves biologically as a more aggressive cancer.”
The researchers’ data show that the use of RAI has gone up significantly in the U.S. in the past four decades from about 5 percent in 1973 to 50 percent in 2016. “That’s a staggering increase,” Dr. Mukherjee says.
The incidence of WDTC also increased significantly during that period, but Dr. Mukherjee says that increase is due mainly to increased ultrasound detection of low-risk tumors.
“There is a concern of overdiagnosis of WDTC tumors and potential overtreatment with RAI, and recommendations against routine use of RAI in WDTC patients with low-risk disease and some intermediate-risk disease,” says Dr. Mukherjee.
Advertisement
“What our data suggest is that giving radioactive iodine is not without any risk. There is a risk of leukemia, even though the risk is small, and it may be potentially avoidable.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting