Managing CF at home is possible, but steps must be taken by both patient and caregiver
Although COVID-19 poses a major risk to all patients, those with cystic fibrosis (CF) may be at a particularly high risk of death should they be hospitalized with COVID-19, according to expert opinion. Appearing in Cleveland Clinic Journal of Medicine’s collection of COVID-19 Curbside Consults, a commentary from Elliot Dasenbrook, MD outlines best care practices for this patient population in the midst of the pandemic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Dasenbrook says that the principal care strategy for CF patients is to keep hospitalization as a last resort. He notes that there are a few strategies that can be used for outpatient management.
Telemedicine can give CF patients needed care without increasing infection risk. Home spirometers, pulse oximeters and mailing sputum samples to the clinic can help provide caregivers with the data they need while at the same time maintaining social distancing for their vulnerable patients. Communication with patients is vital and can be done through a variety of channels. Video-sessions, eblasts and social media can all be used to provide information and updates to patients about COVID-19. Caregivers can also use these tools to notify patients of any pandemic-related changes at their CF center.
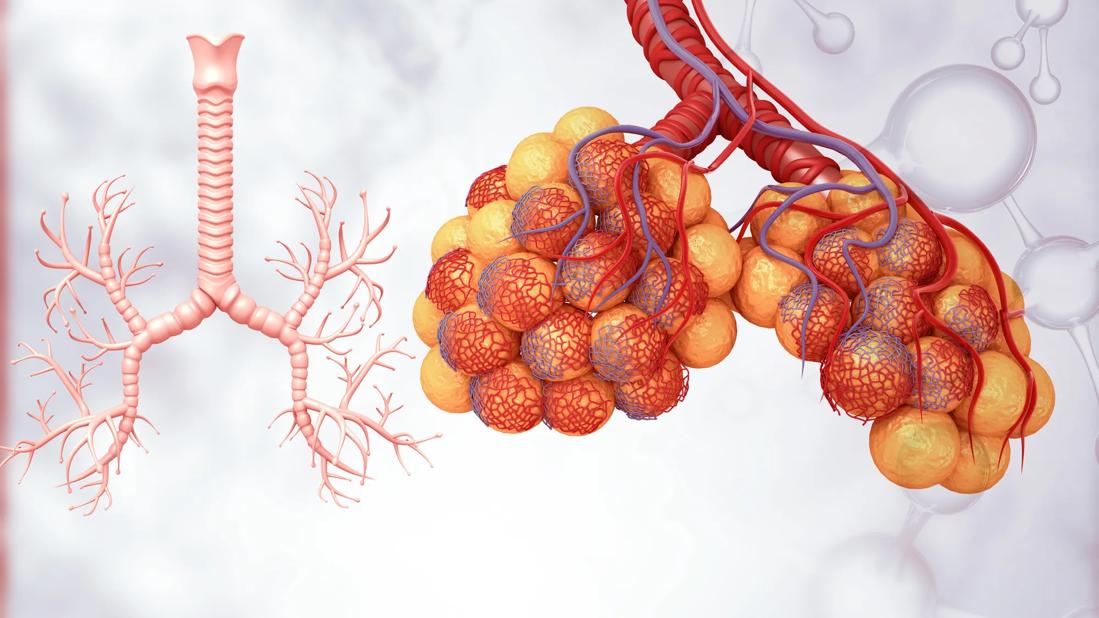
Aggressive treatment of CF exacerbations is also important in preventing the need for hospitalization. Increased airway clearance methods and antibiotics are the best regimens. When possible, a course of intravenous antibiotics at home should be considered for more severe pulmonary exacerbations. Elexacaftor-tezacaftor-ivacaftor is a combination medication targeting specifically the genetic processes that lead to CF. It has resulted in a significant reduction in pulmonary exacerbation among CF patients. Many CF centers have, anecdotally, noticed fewer hospitalizations since its introduction in October 2019, and this reduction may prove to be of even greater value during the COVID-19 pandemic.
Advertisement
A caregiver may have also prescribed strategies to a patient to help him or her maintain lung health. It is important to reinforce adherence to these regimens, such as exercise, airway clearance, anti-inflammatory drugs, antibiotics and modulator therapy.
Two treatment options for CF patients with questions surrounding them because of COVID-19 are ibuprofen and corticosteroids. While much of the data is anecdotal, there is no strong link between worse outcomes in COVID-19 and ibuprofen. But acetaminophen can be used instead of ibuprofen for the sake of caution. Patients who have been treated for CF lung disease with high-dose ibuprofen can continue their treatment plan, but patients should be reassessed on a case-by-case basis.
Data on corticosteroids and COVID-19 are from the critically ill, so CF patients with asthma or allergic bronchopulmonary aspergillosis who require oral or injected corticosteroids should continue at the lowest possible dose to maintain their health.
In his commentary, Dr. Dasenbrook also describes treatment plans for CF patients who must be hospitalized. This information, along with the full article from Cleveland Clinic Journal of Medicine’s COVID-19 Curbside Consults, a list of resources and references, can be found here.
Advertisement
Advertisement

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition

As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19