Nintedanib significantly reduces loss of lung function
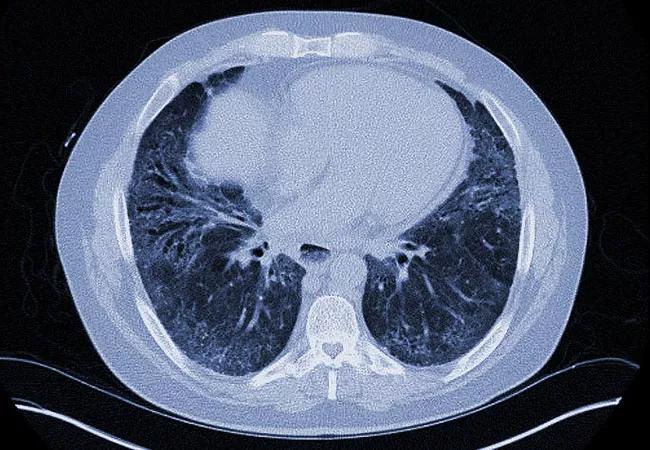
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/32cc7d56-5c30-418f-9791-a5625473cdbe/650x450-Scleroderma-NSIP_jpg)
650×450-Scleroderma-NSIP
Results from a just-published landmark trial could lead to the first-ever approved drug for the treatment of systemic scleroderma-associated interstitial lung disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Systemic sclerosis (SSc) is a relatively rare, heterogeneous autoimmune disease characterized by immune dysregulation, microvascular damage and organ fibrosis. About 40% of SSc patients experience interstitial lung disease (ILD), a major cause of morbidity and mortality.
The intracellular tyrosine kinase inhibitor nintedanib significantly reduced the loss of lung function in the 52-week, randomized, double-blind, placebo-controlled Safety and Efficacy of Nintedanib in Systemic SClerosIS (SENSCIS) trial. The trial involved nearly 600 patients in 32 countries. The drug has been FDA-approved for the treatment of idiopathic pulmonary fibrosis (IPF) since 2014.
Although the majority of patients in the SENSCIS study did not have an improvement in lung function, the decreased rate of decline in pulmonary function compared to placebo was clinically significant.
“Nintedanib adds to our treatment armamentarium,” says co-lead investigator Kristin Highland, MD, Director of Cleveland Clinic’s rheumatic lung disease program. “We now have the option of targeting multiple important pathways in scleroderma, with nintedanib targeting the fibrotic pathway and off-label immunosuppressive treatments targeting immune dysregulation.
“This drug isn’t likely to make anyone feel better, but for people who are young and have ILD related to scleroderma and wonder if they’re going to be around to see their children grow up, this drug could increase the chances of that happening because there’s a slower rate of decline in their lung function. We didn’t prove a mortality benefit in this study, but that would be the potential implication.”
Advertisement
Gastrointestinal (GI) adverse events were more common with nintedanib than placebo, but they were no worse than what IPF patients experience. This finding was reassuring, given that scleroderma itself is associated with GI toxicity, including reflux and diarrhea, which are not as prevalent in IPF. Additionally, many subjects enrolled in the trial were on background mycophenolate, which also can cause diarrhea.
The reason for the lack of additive GI toxicity isn’t clear.
“We can only theorize, but if you have fibrosis of the GI system, maybe nintedanib was helping,” says Dr. Highland.
Dr. Highland and co-lead author Oliver Distler, MD, of University Hospital Zurich, presented the SENSCIS findings at the 2019 American Thoracic Society annual meeting in Dallas. The results were simultaneously published in The New England Journal of Medicine.
A total of 576 patients with SSc were treated in the study, including 51.9% with diffuse cutaneous SSc and 48.4% who were taking mycophenolate at baseline. All had onset of their first non-Raynaud symptom within the past seven years and at least 10% fibrosis of the lungs on high-resolution computed tomography scan.
They were randomized 1:1 to either 150 mg oral nintedanib twice daily or placebo.
The adjusted annual rate of decline in forced vital capacity (FVC) assessed over 52 weeks — the primary endpoint — was -52.4 ml/year with nintedanib versus -93.3 ml/year with placebo (P = 0.04).
Among the secondary endpoints, there were no significant differences between nintedanib and placebo in change from baseline in the modified Rodnan skin score or the St. George’s Respiratory Questionnaire total score.
Advertisement
Since prior animal studies had suggested improvements in skin manifestations with nintedanib, Dr. Highland suspects that the reason for the lack of effect may have to do with variation in the way the Rodnan score was administered across countries.
“I think we should wait and see what the biopsy substudy shows,” she says.
Adverse events leading to discontinuation were more common in the nintedanib group (16.0%) than with placebo (8.7%). Diarrhea was reported in 75.7% and 31.6%, respectively. Deaths occurred in 3.5% versus 3.1%, respectively, not a significant difference.
The potential for this drug to become FDA-approved would make a huge difference to scleroderma patients and physicians, Dr. Highland believes.
“It would give doctors a brand-new tool,” she says. “There are no FDA-approved therapies for scleroderma right now. Every single drug we want to use is off-label, requires pre-authorization, and is difficult to get our hands on. It would be a relief to have something on-label for this horrible disease.”
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program