Large series finds outcomes from staged “endo-open” strategy comparable to open repair

Treating extensive aortic aneurysm disease with descending thoracic aorta stent grafting followed by distal open completion — so-called staged ultra-hybrid repair — can yield outcomes comparable to those with open thoracoabdominal aortic aneurysm (TAAA) repair in a very high-risk population. So concludes an analysis of 92 patients who underwent completion of the hybrid procedure at Cleveland Clinic in the largest reported series to date, published in Seminars in Thoracic and Cardiovascular Surgery (2022;S1043-0679(22)00256-8).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Patients selected for this strategy often have pan-aortic disease extending beyond a thoracoabdominal aneurysm, sometimes with a genetic syndrome leading to complex anatomies due to chronic dissection,” says the study’s senior author, Eric Roselli, MD, Chief of Adult Cardiac Surgery at Cleveland Clinic. “The majority of the patients underwent multiple stages of repair, including prior root, ascending and total arch replacements with a first-stage elephant trunk procedure followed again by stent grafting and then completion open repair. A hybrid approach eliminates the need for hypothermic circulatory arrest and limits left lung manipulation and spinal cord ischemia by breaking up a total aortic repair into additional stages.”
“Ultra-hybrid repair was born out of patients surviving so well after being treated for aortic dissection with a stent graft,” adds co-author Francis Caputo, MD, Vascular Surgery Director of Cleveland Clinic’s Aorta Center. “Those who develop progressive aneurysmal degeneration distal to the thoracic stent can benefit from a subsequent open operation to complete the repair.”
The ultra-hybrid approach consists of initial proximal thoracic aortic repair, descending thoracic aortic stent grafting and open distal repair across the thoracoabdominal segment at some point (days to years) afterwards. Compared with fully open repair — traditionally regarded as the “gold standard” — the hybrid approach may be associated with lower mortality and possibly a reduced risk of spinal cord injury.
Advertisement
Cleveland Clinic cardiac and vascular surgeons have increasingly adopted the ultra-hybrid strategy over the past 15 years, with numbers doubling from 2020 (19 cases) to 2021 (38 cases). The current series analysis shares their experience in terms of patient population, operative techniques and outcomes.
The series included 92 adults (68% men; mean age, 58 ± 13 years) who completed a staged, hybrid TAAA repair between 2006 and 2020. Of these, 46% had a planned second stage, i.e., completion within six months of thoracic stent grafting. Over one-third of patients had a known or suspected heritable aortic condition.
Descending thoracic stent grafting was performed as a conventional thoracic endovascular aortic repair in 75% of cases and frozen elephant trunk in 5% of cases; another 20% had both, with the first-stage elephant trunk extended by thoracic endovascular aortic repair (TEVAR).
The median interval between stent grafting and open completion was 96 days in patients who underwent planned ultra-hybrid repair and 2.4 years in those who underwent delayed completion. At the time of open TAAA repair, aortic morphology included the following as the primary indication for completion:
After ultra-hybrid repair completion, survival was 80% at one year and 66% at five years. Hospital mortality was 7.6% (n = 7) and was associated with elevated blood urea nitrogen (> 20 mg/dL) and longer distance between the distal endograft edge and the most proximal patent visceral vessel (> 9 cm).
Advertisement
Complications included acute renal failure requiring dialysis (incidence of 20%), tracheostomy (8.7%), permanent paralysis (6.9%) and stroke (5.7%).
Freedom from aortic or iliac reoperation was 86% at one year and 66% at four years. Larger iliac diameter (> 2 cm) increased the risk of needing reoperation, often on the aortic bifurcation and iliac vessels.
In their study report, the authors emphasize that the findings from their experience in these ultra-hybrid completion operations highlight the importance of multidisciplinary care and treatment strategies directed at a lifelong approach for aortic disease.
“A staged repair strategy for patients at risk for progressive aneurysmal degeneration can limit overall risk by minimizing the burden of trauma at any one stage,” says Dr. Roselli. He notes that the hybrid approach can be applied to those in need of repair distal to a preexisting thoracic endograft, as well as to patients with TAAAs deemed to be high risk for a single-stage operation or those not anatomically amenable to a purely endovascular repair. “This strategy also offers advantages to patients with moderate lung compromise and those who had previous open surgery in their left chest,” he adds, “as it limits the impact of open surgery to the more distal aorta.”
Drs. Roselli, Caputo and their co-authors provide the following insights from the Cleveland Clinic experience:
Advertisement
“The number of ultra-hybrid repairs we perform is steadily increasing as our referrals grow and the procedure becomes more standardized,” says Dr. Roselli. “We are constantly striving to improve results and are now refining graft design by adding a proximal cuff to better facilitate the endograft-to-surgical graft interface.”
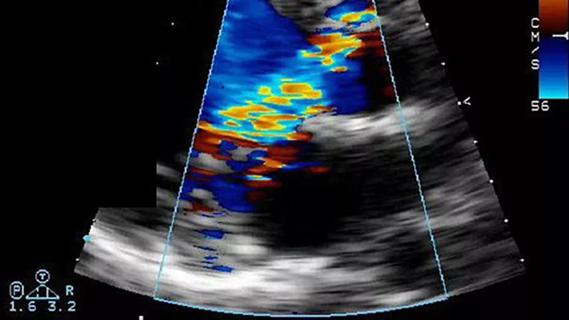
Image at top: Successive stages of the ultra-hybrid approach to TAAA repair.
Advertisement
Advertisement

New Cleveland Clinic data challenge traditional size thresholds for surgical intervention

Study finds comparable midterm safety outcomes, suggesting anatomy and surgeon preference should drive choice

New review distills insights and best practices from a high-volume center

Blood test can identify patients who need more frequent monitoring or earlier surgery to prevent dissection or rupture

Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR

Multicenter pivotal study may lead to first endovascular treatment for the ascending aorta
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Large cohort study finds significant effect in men and nonsmokers