Surgeons credit good outcomes to experience with complex cases and team approach
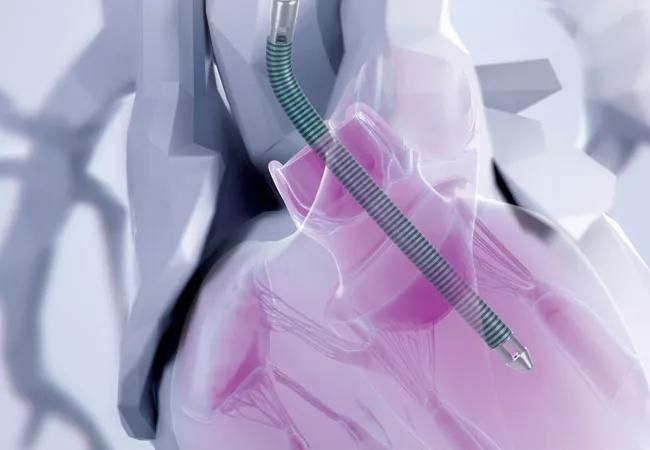
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fe291c37-ce6c-4990-8a07-bf26bd62352e/20-HVI-2034260_impella-heart-illustration_650x450_jpg)
pointy medical device entering chambers of the heart through a major vessel
Surgical aortic valve replacement (SAVR) can be a major operation for any patient if compounded by factors such as reoperation, low ejection fraction or the concomitant need for other procedures, such as mitral valve repair/replacement or coronary artery bypass grafting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“As a high-volume center with long experience handling complex cardiovascular cases, Cleveland Clinic is at the forefront of developing surgical techniques and management strategies for high-risk aortic valve replacement,” says Edward Soltesz, MD, MPH, Surgical Director of Cleveland Clinic’s Kaufman Center for Heart Failure Treatment and Recovery. “We are able to achieve excellent outcomes for many patients who are deemed too high risk for surgery, including SAVR, at other hospitals.”
Cardiac Consult checked in with Dr. Soltesz and his Cleveland Clinic cardiothoracic surgery colleague Haytham Elgharably, MD, to explore two key areas relevant to more than a few SAVR cases: concomitant additional valve repair or replacement, and the use of preemptive microaxial temporary left ventricular assist device (LVAD) support for patients at high risk of postoperative cardiogenic shock.
Dr. Elgharably has developed a specialty interest in multivalve operations, either as initial surgery or in the reoperative setting, often resulting from a failed or mismatched aortic valve prosthesis. “These are technically demanding surgeries that can involve multiple components,” Dr. Elgharably notes. He adds that the patient may have been operated on more than once previously, compounding the challenges.
The Cleveland Clinic surgical team recently reported on over 2,300 reoperations involving replacement or repair of multiple heart valves between 2008 and 2022 (J Thorac Cardiovasc Surg. 2024;168[6]:1632-1642), more than half of which included SAVR as a component. Overall outcomes included 3.9% hospital mortality and 4.2% operative mortality. Elective isolated multivalve reoperations — i.e., without additional procedures such as aorta surgery or coronary bypass — had lower mortality rates (1.6% hospital and 1.7% operative). Factors that increased risk included preoperative end-organ dysfunction and additional surgical components, especially coronary artery bypass grafting.
Advertisement
“We need to tailor our surgical approach to each patient based on their cardiac pathology, clinical presentation and comorbidities,” Dr. Elgharably says. “Yet regardless of the complexity of the operation, simply adding more time on the bypass machine increases risk, which must also be considered.”
He nevertheless acknowledges the importance of addressing problems that are not likely to improve on their own simply after replacing the aortic valve, such as a leaky mitral valve or stenotic coronary arteries. He identifies the following as instances when complex multivalve surgery may be indicated:
Advertisement
“Many factors are critical to success in these complex cases,” says Dr. Elgharably. “These include thorough preoperative assessment of the heart and proper sizing of the replacement valves, as well as preoperative evaluation of lung, liver and other organ status. Outcomes are optimized when a team of specialists can closely collaborate on determining strategy and patient management.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3e794228-3f15-4954-a882-d590b167d2c8/23-HVI-3655709-Inset-2_jpg)
Figure. Operative photo showing a Commando exposure. Asc Ao = ascending aorta; LVOT = left ventricular outflow tract; LA = left atrium; RA = right atrium; RV = right ventricle.
“Whenever approaching a patient with low ejection fraction — or any patient about to undergo complex cardiac surgery — having a strategy in place to support the heart in the first few days after surgery is of utmost importance,” says Dr. Soltesz, who has published several papers with Cleveland Clinic colleagues on the preemptive use of a percutaneous ventricular assist device (pVAD) for high-risk patients undergoing cardiac surgery.
He notes that preemptive use of such support appears to be crucial. “Waiting for cardiogenic shock to develop and then reacting with pVAD insertion is associated with very high mortality,” he says.
Dr. Soltesz is national co-principal investigator of the multicenter, prospective single-arm IMPACT trial (NCT05529654), which is evaluating the preemptive use of pVAD support for cardiac surgery in patients with low ejection fraction, as detailed in a recent Consult QD post. Results are expected in late 2025.
He adds that defining which patients are likely to develop postoperative cardiogenic shock — and would therefore most benefit from preemptive device placement — is an important area of ongoing research. A recent study in the Journal of Thoracic and Cardiovascular Surgery (2024;168[5]:1489-1499) examined Cleveland Clinic data and found that baseline predictors of postoperative cardiogenic shock differed between patients with ischemic cardiomyopathy (in whom right heart dysfunction, indicated by low pulmonary artery pulsatility index, was the most important) versus nonischemic cardiomyopathy (in whom greater cardiac decompensation was most important).
Advertisement
Dr. Soltesz emphasizes that for complex cardiac surgery, including SAVR in high-risk settings, engaging in a shared decision-making process with patients is essential. “We need to thoroughly discuss with the patient their goals and what can be expected from the various treatment strategies,” he says. “Patients usually have strong opinions about the amount of risk they are willing to take on.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
For many patients, repair is feasible, durable and preferred over replacement
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach
20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation