30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
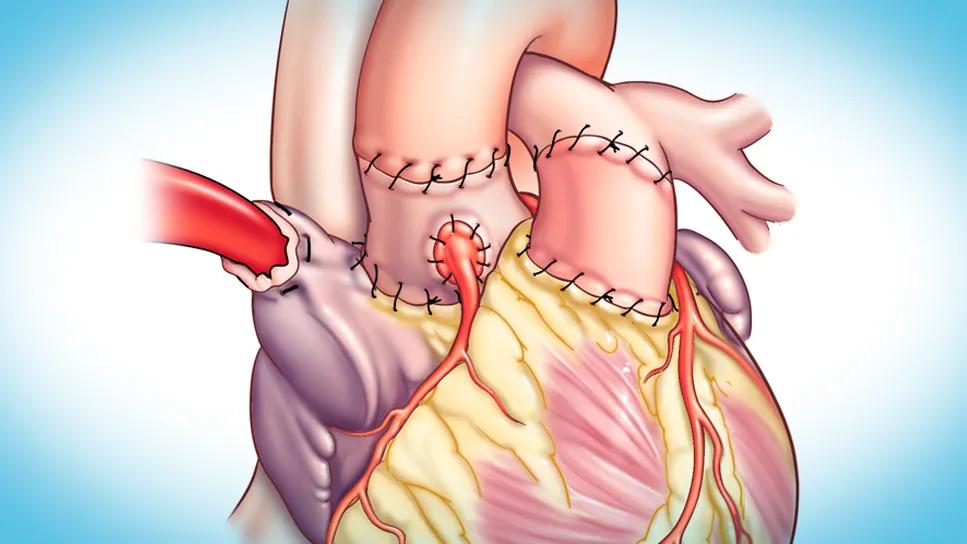
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3587a2a6-1159-4f9d-a12e-f373e9e2f9e1/25-HVI-6143858-CQD)
heart with a grafted vein to the aorta
The Ross procedure can be a good strategy for young adults with aortic valve disease, offering advantages over other procedures for aortic valve replacement (AVR) and resulting in favorable long-term clinical and quality-of life (QOL) outcomes. So confirmed a longitudinal study of 166 patients who underwent the procedure at Cleveland Clinic over a 30-year period (Ann Thorac Surg. 2025 Epub 3 Mar). Notably, the analysis showed that patients having surgery after the year 2000 experienced better results than those in the previous decade.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Many surgeons have shied away from the Ross procedure because of reports of complications during the 1990s and the potential need for reintervention for two valves,” says Cleveland Clinic cardiac surgeon Shinya Unai, MD, a study author. “However, improved surgical approach, patient selection and postoperative management over the years have made it a compelling option for AVR, especially for young adults.”
Compared with other treatments for AVR, the Ross procedure offers excellent hemodynamics and a low risk of thromboembolism and endocarditis. Disadvantages associated with other common surgical AVR options — e.g., the need for lifelong anticoagulation with a mechanical valve and deterioration of a bioprosthetic valve over time — are reduced (see recent Consult QD article profiling AVR options).
“It is critical that we tailor valve choice to the specifics of a patient’s disease, their personal quality-of-life considerations and our own technical expertise as providers,” says Eric Roselli, MD, Chief of Adult Cardiac Surgery at Cleveland Clinic and a proponent of the Ross procedure. “This is optimized by embracing a shared decision-making approach with our patients, as well as continuous review of results to improve our outcomes.”
The 2020 American College of Cardiology/American Heart Association valve guidelines gave the Ross procedure a weak recommendation (Class IIB) due to insufficient evidence. The new study examining the Cleveland Clinic experience with the Ross procedure over 30 years, with a focus on long-term clinical and patient-reported outcomes, provides additional data to inform future guidelines.
Advertisement
The Ross procedure is a complex operation, involving removal of the diseased aortic valve, replacement of the aortic valve with the patient’s healthy pulmonary valve (PV) and implantation of a PV donor homograft in the PV position. The coronary arteries disconnected from the aortic root are reimplanted onto the autograft.
Multiple changes to the Ross procedure occurred at Cleveland Clinic starting in the year 2000, emphasizing standardization of patient selection and improved surgical techniques. Standardization around patient selection favored patients younger than 55 with optimal preoperative function, isolated aortic stenosis or mixed aortic stenosis/aortic regurgitation, and controlled hypertension. Bicuspid stenotic valves are not disqualifying, but root enlargement and aortic valve regurgitation, including from bicuspid valves, are a disqualifier.
The improvements in surgical technique included use of a buttressing approach, preserving the native root and circumferentially wrapping the autograft, plicating the annulus, and using a short interposition ascending graft for stabilization. Also, follow-up protocols now include strict blood pressure control to reduce aortic wall stress and promote autograft success.
“In recent years,” Dr. Roselli notes, “we have further refined the Ross options to include a supported Ross variation where the autograft is stabilized within a prosthetic graft for patients with even more complex presentations. Success with this is based on our experience with rescuing failing autografts.” (Learn more in this video with Dr. Roselli: youtube.com/watch?v=8na6CP5ji-E.)
Advertisement
Patients who underwent the Ross procedure at Cleveland Clinic between January 1990 and April 2021 were included in the study (N = 166; n = 73 before and n = 93 after the year 2000). Patients were aged 14 to 63 years (mean of 32); 71% were male.
Median follow-up was 7.3 years postoperatively, with 25% of patients followed for more than 19 years and 10% for longer than 27 years.
Overall survival was 94% at 10 years and 70% at 25 years. No deaths occurred in patients undergoing surgery after the year 2000. Two patients had strokes, each about five years postoperatively. No bleeding events were reported during follow-up.
In patients who underwent surgery after 2000, long-term autograft valve mean gradients remained low (average of 4.4 mm Hg at 20 years) and 10-year freedom from all reintervention was 96%. Reinterventions were more likely to occur in socially disadvantaged patients.
“We also emphasized self-reported quality-of-life assessment, as most modern aortic valve interventions have similar objective clinical outcomes,” Dr. Unai notes. “QOL comes to the fore in decision-making for a young patient.”
QOL assessment was performed with PROMIS-10 and MacNew surveys: 82 patients completed them, at a median of 9.4 years postoperatively. Survey responders were more likely to have had more recent surgery and fewer comorbidities.
Results included the following:
Advertisement
Female sex, reintervention and older age at surgery/assessment were associated with poorer scores in many of the QOL categories. Notably, overall patients with biological valves scored higher than patients with Ross procedures in a matched analysis at 15 years.
The study authors offer the following advice to institutions offering the Ross procedure:
“We now have enough experience with the Ross procedure to recognize its benefits and potential pitfalls,” Dr. Unai observes. “With changes instituted in recent decades, we feel comfortable offering it to many younger adults needing aortic valve replacement.”
“Cleveland Clinic’s experience with the Ross procedure adds meaningful evidence to the ongoing discussion around optimal aortic valve replacement strategies in younger adults,” says Serge Harb, MD, a Cleveland Clinic cardiologist specializing in valvular heart disease. “From a cardiology standpoint, the Ross procedure offers compelling hemodynamic performance and avoids the need for lifelong anticoagulation, which is a major consideration for many young patients.
“What stands out in this series,” Dr. Harb continues, “is the emphasis on patient-centered outcomes, particularly quality of life, which is an increasingly central component of decision-making in this age group.
Advertisement
“These data underscore the value of multidisciplinary collaboration and experienced center expertise in offering the Ross procedure to carefully selected patients,” Dr. Harb concludes. “In this context, shared decision-making becomes not just ideal but essential.”
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
Surgeons credit good outcomes to experience with complex cases and team approach
For many patients, repair is feasible, durable and preferred over replacement
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach
20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation