Physician experience refines patient selection criteria for endoscopic lung volume reduction
Four years ago, the FDA approved the first valve system for endoscopic lung volume reduction (eLVR), a minimally invasive alternative to surgical lung reduction for patients with severe chronic obstructive pulmonary disease (COPD) or advanced emphysema. Less than two years later, endobronchial valve therapy was included in the 2020 update of the Global Initiative for Chronic Obstructive Lung Disease with an “A” evidence level rating.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Growing physician experience with valve therapy is helping refine patient selection, a key element for achieving positive outcomes,” says Diego Maldonado, MD, FCCP, an interventional pulmonologist with Cleveland Clinic Indian River Hospital, where the treatment has been available since 2019.
Today approximately 15 million Americans are living with COPD, according to the Centers for Disease Control and Prevention. Severe COPD is characterized by reduced lung recoil and expiratory flow, increased air trapping, and hyperinflation. On pulmonary function tests it appears as increased residual volume and total lung capacity.
“Hyperinflation puts added pressure on the diaphragm and intercostal muscles, raises intrathoracic pressure, and decreases cardiac filling,” explains Dr. Maldonado. “That results in dyspnea and reduced exercise tolerance with subsequent quality of life impacts.”
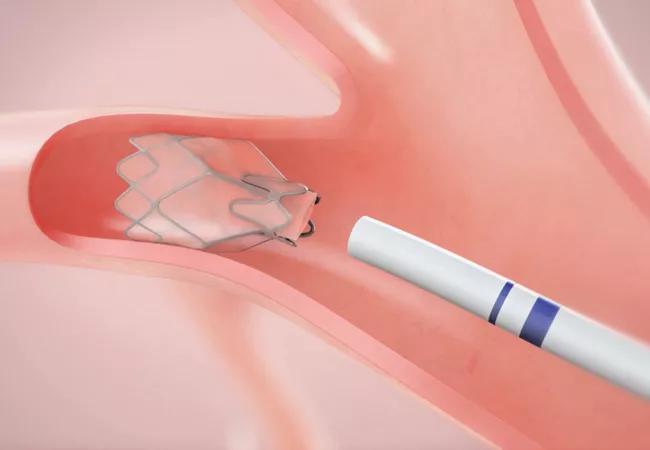
During endobronchial valve therapy, an average of one to four tiny valves are placed in the airways to achieve lobar atelectasis. By preventing air from being trapped in the most diseased area of the lung, healthier sections can take in more air, lifting pressure off the diaphragm.
“Valve therapy is far less invasive than surgical lung volume reduction, it’s reversible, and patients experience fewer side effects including less pain, a shorter hospital stay, and a lower mortality rate,” notes Dr. Maldonado.
Software analysis is used to identify the target lobe with the highest emphysema destruction score, the least contribution to gas exchange, and a greater than 10% to 15% difference compared with the neighboring lobe. Fissure integrity is also assessed, as it is an essential criterion needed to ensure treatment success.
Advertisement
“We take a conversative approach by only treating one lobe at a time,” says Dr. Maldonado. “If necessary, we can go back and collapse a second lobe to achieve a greater response or to address disease progression.”
Valve therapy is approved for patients with severe obstruction, hyperinflation, and air trapping and with no collateral ventilation. It provides symptom relief for patients with heterogeneous emphysema who have not sufficiently responded to other treatments including tobacco cessation, immunization, pulmonary rehabilitation, and medication management.
“Patients with stage three or four COPD and a residual volume of 170 or greater are potential candidates but not everyone will qualify,” emphasizes Ivan Romero-Legro, MD, an interventional pulmonologist with Cleveland Clinic Weston Hospital, where the procedure is also offered. He notes in one multicenter randomized controlled trial, only 190 out of 909 patients with heterogeneous emphysema qualified for the procedure.
“Based on studies and our early experience, we know there are certain disease characteristics that are less likely to achieve good results with this treatment approach,” says Dr. Romero-Legro, who has treated more than 50 patients with eLVR. “These include chronic bronchitis, frequent infections, and bronchiectasis.”
Other contraindications to valve therapy include:
Advertisement
The screening process to identify candidates for endobronchial valve therapy begins with a pulmonary function test and 6-minute walk test. A chest CT is performed to check for lung masses and to assess fissure integrity. An echocardiogram is also performed to rule out pulmonary hypertension.
“Lack of fissure integrity between lobes is one of the most common disqualifiers for valve therapy because it indicates the presence of collateral ventilation,” says Dr. Romero-Legro. “But many of these patients remain candidates for lung volume reduction surgery.”
If a patient qualifies for eLVR, a final test called the Chartis procedure is performed during the bronchoscopy before valve placement. It entails occluding the target airway with a balloon catheter that only allows expiratory airflow. Continuous expiratory airflow after occlusion indicates the presence of collateral ventilation, which nullifies lung volume reduction.
Primary care providers should consider referral for endoscopic lung volume reduction for patients with severe emphysema and poor quality of life despite optimal pharmacologic treatment and pulmonary rehabilitation.
“For some qualifying patients, the results can be quite dramatic,” adds Dr. Maldonado, recalling one of his first patients, a woman in her mid-60s with severe shortness of breath and hyperinflation, who had difficulty talking and walking.
“She had one of the fastest treatment responses and no longer needs continuous oxygen,” he says, noting at the three-month follow-up visit the patient was laughing and walking with ease. “She continues to benefit from the results of the procedure three years later.”
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.