An underappreciated immune-related adverse event
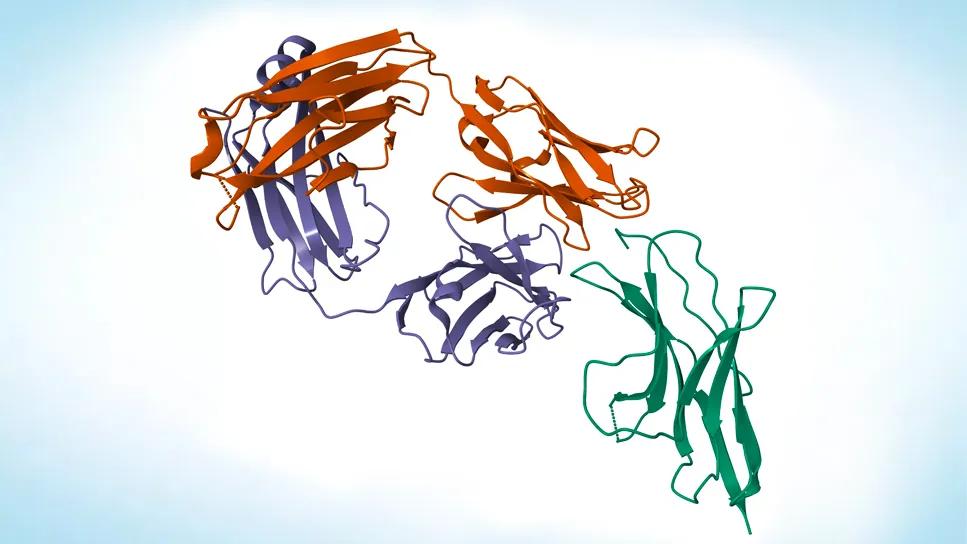
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fefddb4f-892f-4dbd-8b5c-9dd5ae91a019/tumor-immunotherapy-with-nivolumab-2174311608)
Nivolumab
Venous thromboembolism (VTE) occurs in up to 25% of cancer patients treated with immunotherapy, according to a Cleveland Clinic study published recently in Med. Researchers also identified potential biomarkers that can assist in stratifying patients’ risk of VTE when treated with immunotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The impact of immunotherapy on cancer prognosis for many patients cannot be understated,” says Keith R. McCrae, MD, Director of Benign Hematology at Cleveland Clinic Cancer Center and coauthor of the study, “but neither can the potential for and prevalence of immune-related adverse events. Our results show that VTE should be considered a common toxicity of cancer immunotherapy.”
The study was part of a $4.7 million grant from the National Heart, Lung and Blood Institute (NHLBI) and led by Dr. McCrae and Alok Khorana, MD, to study the prevention of life-threatening, cancer-associated thrombosis.
This retrospective cohort study included 1,686 patients who were treated with immunotherapy for various malignancies. The mean age was 64.5 years, and most patients were male (60.1%), white (86.8%) and non-Hispanic (96.4%) with metastatic disease (90.3%). Both the incidence and impact on mortality of VTE were tracked.
Nivolumab was the most commonly used therapy, followed by pembrolizumab, atezolizumab, ipilimumab, avelumab and durvalumab. VTE occurred during immunotherapy in 24% of patients and was associated with a significant decrease in overall survival (OS) (hazard ratio, HR = 1.22 [95% confidence interval (CI), 1.06-1.41, P < 0.008). Researchers found no significant difference in rate of VTE among the therapies.
“This was interesting because the majority of malignancies represented in our cohort were not ones normally associated with VTE, like pancreatic cancer,” says Dr. McCrae. “This further suggests a role for the treatment in the development of VTE, rather than the malignancy itself.”
Advertisement
Previous evidence has implied a potential role for cellular immune response, inflammatory cytokine and compliment-mediated inflammation playing a role in the various immune-related adverse events patients can experience after immunotherapy. Researchers analyzed blood samples taken before the start of immunotherapy in a sub-cohort of patients for 51 plasma cytokines and chemokines associated with inflammation. Those who developed VTE (N = 15) had significantly higher pretreatment levels of myeloid-derived suppressor cells (P = 0.0045), soluble vascular cell adhesion protein 1 (P = 0.0385) and interleukin 8 (P = 0.016) than patients who did not develop VTE (N = 10).
The work of Dr. Khorana, Sondra and Stephen Hardis Chair in Oncology Research and Vice-Chair for Faculty Development at Cleveland Clinic Cancer Center, and senior author of the study, previously established the association of VTE with standard cancer therapies. “In this study, we built upon this work to show that the risk continues for our cancer patients, despite advances in therapy,” he says. “This study is also the first to identify potential biomarkers that can help us determine thrombotic risk in patients treated with immunotherapy.”
The CASSINI and AVERT trials demonstrated that prophylactic anticoagulation can prevent VTE in patients with cancer; if data from the present study can be replicated, and safety can be established, prophylactic anticoagulation may also become standard for cancer patients receiving immunotherapy.
Advertisement
“This preliminary study opens the door for further exploration of the connection between immunotherapy and VTE,” notes Dr. McCrae. “If we can predict and then prevent this adverse event in patients receiving immunotherapy, we can reduce morbidity and mortality and provide better overall care for our patients, which is always the goal.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches