Congenital disorders can require lifelong care demanding peds neurosurgery expertise

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
MP is a 28-year-old right-handed man with a past medical history significant for migraines, seizure disorder and complex congenital hydrocephalus secondary to perinatal group B streptococcal infection treated with bifrontal ventriculoperitoneal shunts. He had numerous revisions throughout childhood for mechanical failure and infections, eventually requiring a fourth ventricular shunt in addition to his earlier bilateral ventricular shunts. As he progressed into adulthood, he required multiple neurosurgical interventions by adult neurosurgeons. Upon his most recent admission with a shunt infection, the pediatric neurosurgical team was consulted due to the intricacies of his shunt system and his complex medical history.
Our initial interaction with MP occurred in the setting of Cleveland Clinic’s newly formed Congenital and Transitional Neurosurgical Program, which was developed in a multidisciplinary fashion to address the growing need for specialized neurosurgical care in adults with congenital disorders requiring neurosurgery. Our evaluation involved an individualized approach to his care from a pediatric perspective. This included a thorough and comprehensive review of his diagnoses, their respective etiologies, and past medical and neurosurgical procedures. An integral part of this process, as is often the case for patients with congenital neurosurgical disorders, is the input of key family members and caregivers, who sometimes provide critical information that can impact neurosurgical decision-making.
Advertisement
With this information we embarked on a systematic treatment plan (see Figure 1) that included removal of his complex shunt system (due to infection) and placement of three separate external ventricular drains, each of which was systematically tested for dependency (after the infection cleared) independent of the others.
When MP was ready for his shunt system to be reimplanted, we did so using an antibiotic-impregnated and simplified system that required only two of the three previous components. He was discharged on postoperative day 2. He has since been seen in clinic for his three-month follow-up and remains symptom-free. He is nicely acclimated to his new, less-intricate shunt system.
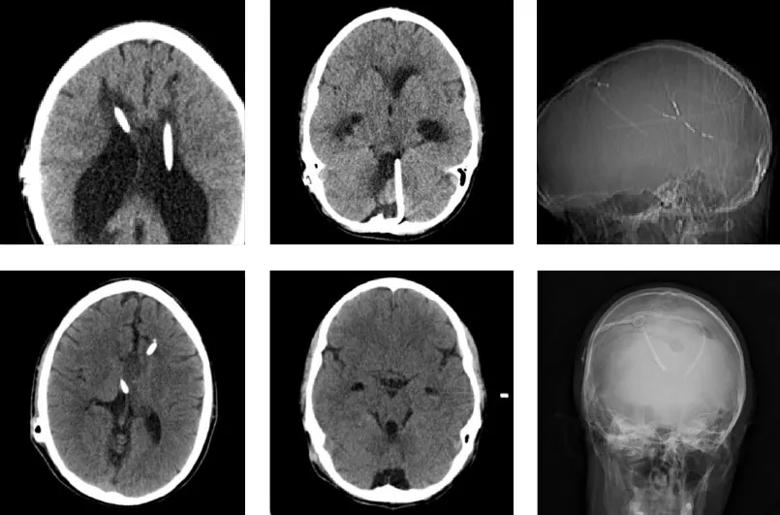
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/45444cfd-7c3c-4f24-a4bc-e2fefc574548/17-NEU-980_Onwuzulike-Recinos-inset1_jpg)
Figure 1. Preoperative (top row) and postoperative (bottom row) imaging studies of the case patient. Top: Left image shows the supratentorial bilateral ventricular shunt system (right frontal and left occipital) in florid failure at presentation. Middle image shows the infratentorial fourth ventricular shunt. Radiograph on the right shows the triple shunt system. Bottom: Left image shows the bilateral frontal ventricular peritoneal shunts postoperatively, with acute hydrocephalus resolved. Middle image shows successful weaning of the fourth ventricular catheter. Radiograph on the right shows the simplified two-catheter system.
The field of pediatric neurosurgery encompasses a variety of diseases first encountered in childhood that often require long-term developmental and postoperative management persisting into adulthood. The degree of independence and underlying developmental delay in an individual can significantly influence the extent of coordinated care required by treatment teams. This case illustrates the importance of transitional neurosurgical programs in the care of adults with pediatric disease that required neurosurgery.
Advertisement
These patients’ ongoing needs have historically been managed insufficiently, causing mounting frustration as well as immeasurable financial burden on the healthcare system. Few programs exist that adequately address the needs of this subgroup of patients, whose care is often quite fragmented. Moreover, with advances in perinatal neurosurgical care, more children with previously untreatable neurological disorders are now surviving into adulthood and require appropriate understanding of the management of their congenital disorders. Compounding these challenges, pediatric neurosurgeons face uncertain reimbursement regulations. The Affordable Care Act has assuaged some of these concerns, but significant work is still needed to optimize the care of this subset of patients.
In response, we have developed a paradigm for the care of these patients as they transition to adulthood, to address unmet needs and provide developmentally appropriate, coordinated care. Given that Cleveland Clinic Children’s operates within the broader Cleveland Clinic health system, with shared resources and electronic records, our care model allows delivery of seamless and well-informed care to these patients from fetal life to adulthood.
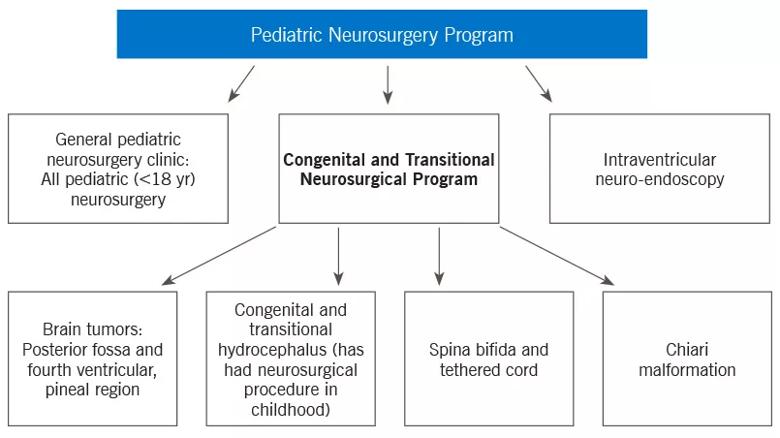
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5c4099f1-52fc-4670-8cf6-4b9233c031ca/17-NEU-980_Onwuzulike-Recinos-inset2_jpg)
Figure 2. Flowchart illustrating the place of the Congenital and Transitional Neurosurgical Program within Cleveland Clinic’s broader pediatric neurosurgery offerings.
Our Congenital and Transitional Neurosurgical Program, which is intended to serve as a national model for transitional neurosurgical care, is founded on two tenets essential to the optimal management of these complex patients:
Advertisement
Dr. Onwuzulike and Dr. Recinos are pediatric neurosurgeons with Cleveland Clinic’s Center for Pediatric Neurosciences.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help