Change in PCV13 recommendations
Starting this year, guidelines from the CDC recommended that all adults over age 65 continue to receive the 23-valent polysaccharide vaccine (PPSV23) to prevent pneumococcal pneumonia. The guidelines changed how the pneumococcal conjugate vaccine is recommended (PCV13). Geriatrician Kenneth Koncilja, MD, discusses the change in this Q&A with ConsultQD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Previously, PCV13 was also recommended for all older adults. Now, the recommendation is for shared decision making between doctor and patient and more selectivity in who receives PCV13. Basically, any older adult with a high-risk chronic medical condition is still is recommended to receive PCV13.
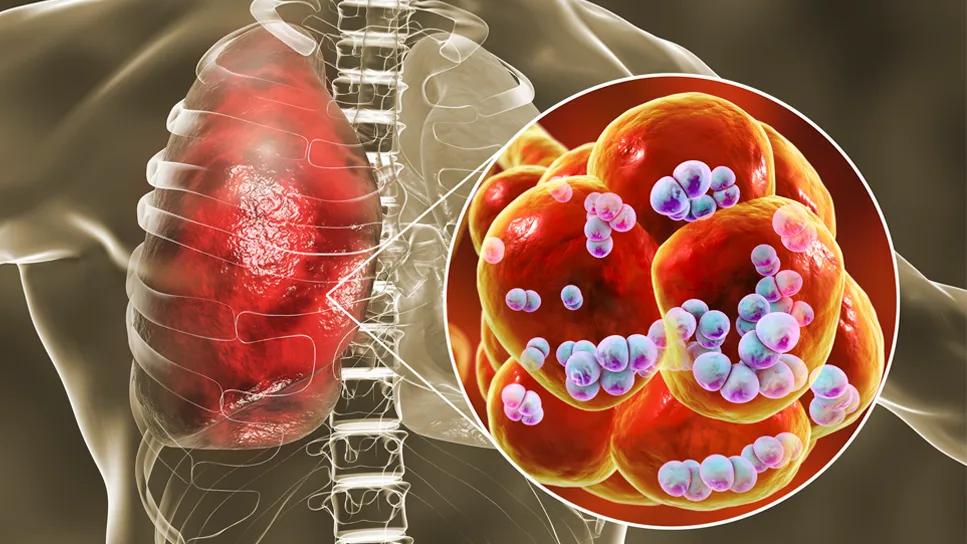
Pneumococcal pneumonia incidence has dropped significantly — ninefold according to the CDC — since PCV13 was introduced in 2010. Specifically, the serotypes of pneumococcus, which reduced, were those covered by PCV13. Children often carry the bacteria, and their continued vaccination has reduced disease burden for older adults. Basically, near universal vaccination of children in the U.S. has reduced exposure for older adults.
The change has given clinicians more flexibility in how we discuss vaccinations. We can prioritize time in the office for the most high-yield disease prevention. For patients, it may be confusing. It’s more difficult to grasp vaccination of another group (children) having such an enormous impact on a different demographic. We need to be more straightforward with patients, and we should be celebrating this as vaccination success.
High risk patients include those:
Advertisement
I like the recommendation to give PVC13 one year before PPSV23; it offers a better immune response. And the good news is that PCV13 is safe with incredibly rare reporting of side effects.
During annual wellness exams is the best time to think about prevention. If patients come in for other reasons, and we have time, I try to address one health maintenance item such as vaccines — including for pneumococcal pneumonia, influenza, zoster or Tdap.
Due to the complexity of patients we face and the care settings we see patients in geriatrics, I am still recommending PCV13 for most of my patients, but I suspect the outcome of less PCV13 serotype pneumonias will continue to improve as vaccination rates in children continue to stay strong.
Yes, the CDC wrote extensively about the decreasing cost-benefit of PCV-13. Essentially, vaccination of all older adults with PCV13 is no longer cost effective as rates of those serotypes continue to decrease.Universal PCV13 was not considered a judicious use of healthcare resources. It’s hard to put money amounts on the benefit of a vaccine; it’s more of a way to compare cost and efficacy with other interventions such as PPSV23.
Advertisement
Advertisement

Researchers explore the mental and physical benefits of social prescribing

Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care

Effective screening, advanced treatments can help preserve quality of life

Study suggests inconsistencies in the emergency department evaluation of geriatric patients

Auditory hallucinations lead to unusual diagnosis

How providers can help prevent and address this under-reported form of abuse

How providers can help older adults protect their assets and personal agency

Recognizing the subtle but destructive signs of psychological abuse in geriatric patients