Progress in stereoelectroencephalography for epilepsy surgery evaluation since Cleveland Clinic performed the first U.S. case in 2009
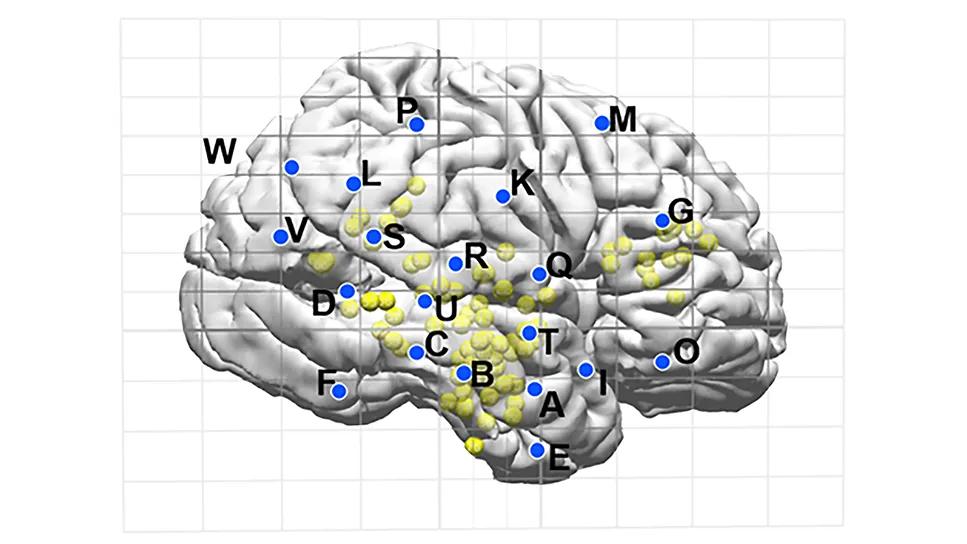
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea57ad06-e088-48e9-a080-e3710d4a9960/learnings-from-1000-seegs)
brain map showing planned electrode placement
In March 2009, Cleveland Clinic performed stereoelectroencephalography (SEEG) on its first patient for localization of seizure foci, becoming the first U.S. institution to use the then-novel minimally invasive technique for implanting depth electrodes. Recently, in August 2024, a Cleveland Clinic Epilepsy Center team performed SEEG evaluation on its 1,000th patient.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Across the intervening 15 years and 1,000 cases, Cleveland Clinic epileptologists and epilepsy surgeons — together with colleagues across the nation and the globe — have refined the application of SEEG in important ways and gained a wealth of insights on its use. Today, Cleveland Clinic uses SEEG in the evaluation of a good proportion of patients referred for epilepsy surgery to treat medically refractory seizures.
Consult QD recently spoke with epileptologist Juan Bulacio, MD, Director of the SEEG program in Cleveland Clinic’s Epilepsy Center, to trace the path of SEEG use across the center’s 1,000 cases and share lessons learned along the way.
More than a quarter century before the adoption of SEEG, capabilities for localizing seizure sources advanced substantially with the advent of subdural grids with depth electrodes. This method allowed physicians for the first time to identify epileptogenic foci and the boundaries of eloquent cortex, but it had definite limitations. Subdural grids require a large incision, a craniotomy and often an extended hospital stay, and they are generally limited to exploration of one brain hemisphere.
Subdural grids with depth electrodes are effective for seizure localization in some settings — patients with identifiable lesions on MRI for whom an anatomo-electrophysiological and functional hypothesis for localization is clear, patients with nonlesional temporal lobe epilepsy, and epilepsy arising from or around the eloquent cortex. Yet there remained important settings in which subdural grids could not meet localization needs, such as patients with nonlesional extratemporal lobe epilepsies (especially if suspected to be frontal) and patients with deep-seated lesions, such as in the depth of a sulcus in an area close to potentially functional cortex.
Advertisement
In the context of these limitations of subdural grids with depth electrodes, Cleveland Clinic epilepsy clinicians began consulting with Italian and French groups pioneering the novel technology of SEEG for medically refractory focal epilepsy. The group — including current Epilepsy Center staff Imad Najm, MD, and William Bingaman, MD, among others — made several trips to Milan and Grenoble from 2004 to 2008 to observe and learn SEEG techniques and processes from the European groups, setting the stage for the first U.S. SEEG case in early 2009.
“We became the earliest U.S. adopter of SEEG in order to achieve better outcomes for patients who are not candidates for subdural grids,” Dr. Bulacio says. “These include patients with bilateral lesions, deep lesions or nonlesional extratemporal lobe epilepsy — what we call MRI-negative cases — particularly in the frontoparietal or frontotemporal regions. SEEG gave us access to areas that are difficult to reach with subdural grids, such as the insula and the cingulate gyrus. It provides a 3D sampling of the brain and allows study of interactions between various network structures that may span multiple lobes or hemispheres to generate seizures. SEEG allows us to study patients with more complex disease.”
Dr. Bulacio views the evolution of SEEG over the ensuing 15 years as breaking down roughly into four periods: the early cases of 2009-2012, expansion of SEEG in 2013-2016, refinements in 2017-2018 and full integration of multimodality imaging from 2019 through the present. Each period saw notable developments in the key areas of SEEG indications, pre-implantation planning and SEEG data analysis.
Advertisement
In these early years, SEEG use was initially limited to confirming the electroclinical hypothesis of seizure localization without sufficiently exploiting SEEG’s potential to identify networks underlying seizure propagation. “We initially tried to tackle problems like we had with subdural grids, which showed a lack of consideration for viewing epilepsy as a network,” Dr. Bulacio explains. “But we soon began to improve upon that and used SEEG with success in patients in whom previous resection had failed, as well as in patients with bilateral electrical findings and deep lesions.”
Pre-implantation planning during this period was informed by discussion at weekly patient management conferences, but the decision of where to place the leads was ultimately made by the treating neurosurgeon. Similarly, data analysis in the early days followed the model of ictal onset interpretation used with subdural grids, which failed to fully capture the diffuse network of onset that can be identified with SEEG. “Ictal onset pattern with SEEG must be interpreted very differently than with subdural grids,” Dr. Bulacio says.
This period saw significant adoption of SEEG by many more U.S. epilepsy centers. By 2013, Cleveland Clinic had expanded its application of SEEG to new indications, including more MRI-negative cases and cases of periventricular nodular heterotopia. Additionally, Epilepsy Center clinicians had adopted by 2013 the network hypothesis for SEEG use — i.e., that seizure generation involves sometimes diffuse networks that can be plotted out for better localization. “SEEG allows us to make an electrical map of the architecture and evolution of the seizure in its onset and spread, even in nonlesional cases,” Dr. Bulacio notes.
Advertisement
Adoption of the network hypothesis had implications for pre-implantation planning. By 2013, planning discussions at the Epilepsy Center’s patient management conferences had yielded far more multidisciplinary decision-making around lead placement.
By this period, the Epilepsy Center team realized that SEEG was not necessary for a group of patients for whom they had been using it: cases of bottom-of-sulcus focal cortical dysplasia (FCD). “Over a series of these cases, we discovered that if various noninvasive studies were concordant on their localization findings, SEEG was not needed,” Dr. Bulacio explains. “That was part of the learning curve.”
This period also saw the emergence of multimodality imaging co-registration to inform pre-implantation planning as well as the ability to translate lead implantation plans to a robotic system to precisely place leads in the brain. SEEG data analysis also advanced. One key development was the introduction of time-frequency analysis, which enabled Epilepsy Center researchers to identify a “fingerprint” of the epileptogenic zone involving a complex pattern encompassing interictal-to-ictal transition (Brain. 2017;141[1]:117-131). Another was the application of signal processing to electrophysiological signals to substantially improve interpretation of SEEG recordings.
The past several years have seen full multimodal image integration into SEEG planning, including SPECT, PET, MEG, EEG and MRI. Additionally, SEEG is increasingly being guided with input from artificial intelligence.
Advertisement
Current indications for SEEG include a large share of MRI-negative cases as well as cases with bilateral abnormalities, large pathologies, periventricular neuronal heterotopia and polymicrogyria-related epilepsy. “Among the latter group of patients, SEEG helped us demonstrate (Seizure. 2024;121:226-234) that not all abnormalities in patients with bilateral or extensive unilateral polymicrogyria need to be resected in order to achieve seizure freedom,” Dr. Bulacio notes.
At the same time, SEEG has been found to not be necessary, if there are concordant findings from noninvasive studies, in cases of encephalocele and FCD 2B in noneloquent cortex (in addition to the earlier discontinuation of SEEG for bottom-of-sulcus FCD).
The collective result of these advances over time has been much more tailored resection. “SEEG allows us to provide the neurosurgeons with the information needed to achieve good outcomes with smaller, more limited resections or with laser ablation,” Dr. Bulacio says.
That has been borne out with data, as reflected in an analysis of seizure outcomes among the first 536 patients who underwent SEEG at Cleveland Clinic from 2009 through the end of 2017 (J Neurosurg. 2022;136:1638-1646). Of these patients, 341 underwent resective surgery, among whom 58% achieved seizure freedom for at least one year, despite the high complexity of cases in the series. Notably, SEEG was found to be comparably effective in patients with frontal and temporal lobe epilepsy and in patients with or without MRI-identified lesions.
“These results show that SEEG has allowed us to achieve good outcomes in patients who don’t fare so well after subdural grid evaluation — those with frontal lobe epilepsy and those with negative MRI findings,” Dr. Bulacio notes. “And this was achieved among our earliest cases, even before some of the more recent enhancements in SEEG use we’ve adopted.” He is currently preparing a similar analysis of outcomes among Cleveland Clinic’s first 1,000 SEEG cases.
SEEG also adds value by better informing decisions to avoid resection in patients deemed to have a poor prognosis. And it helps better identify which patients who are not candidates for resection are likely to benefit from other treatment options, such as neuromodulation. “Post-SEEG use of focal ablation and neuromodulation has increased dramatically in the past decade, and SEEG findings help guide these procedures too,” Dr. Bulacio says. “SEEG is not just improving the diagnosis; it’s also expanding treatment options for many patients.”
He adds that experience at Cleveland Clinic and elsewhere has shown SEEG evaluation itself to be safer than subdural grid evaluation, likely because of its reduced invasiveness. “SEEG is associated with fewer complications,” he says.
When asked to look back over the past 15 years and 1,000 cases, Dr. Bulacio says the most striking advancement has not been in SEEG technology but rather in SEEG methodology. “We have advanced in generating hypotheses about epilepsy networks, which we then confirm or rule out with SEEG,” he explains. “The thing that would have most surprised my former self from 15 years ago is how we can now study the brain to identify epileptogenic networks in very difficult-to-assess regions of the brain such as the cingulate and insula.”
When asked what potential future developments in the field he finds most exciting, Dr. Bulacio’s response is more surprising. “What’s most exciting,” he says, “is the prospect of a future where SEEG is no longer needed. Although it is less invasive than subdural grids, SEEG is still an intracranial evaluation. I would like to be able to learn solely from noninvasive techniques — MRI, studies with other modalities, genetics — everything we need to do the same surgeries that are now guided by SEEG. We’re certainly not there yet, but that can be an ultimate goal.”
Advertisement
Insights on how stereoelectroencephalography is continuing to improve seizure localization
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Comorbidities and medical complexity underlie far more deaths than SUDEP does
Novel Cleveland Clinic project is fueled by a $1 million NIH grant
Paired blood and brain tissue methylation findings raise prospect of noninvasive precision diagnosis
Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline
Researchers pair quantitative imaging with AI to improve surgical outcomes in nonlesional epilepsy