AUA guideline offers specific criteria for deciding between partial versus radical nephrectomy

When the American Urological Association (AUA) published an updated guideline on “Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-up” in 2021, it became the first clinical guideline to define specific criteria for determining radical versus partial nephrectomy in the management of localized renal masses and cancers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Still, questions and controversies remain about choosing a surgical approach that balances functional outcomes with overall survival based on patient-specific factors. And while a partial nephrectomy is generally preferred in this era, when should a radical nephrectomy be considered?
“There’s nothing more controversial in the field of localized kidney cancer than decisions about who should get a partial and who should get a radical nephrectomy,” remarks Steven Campbell, MD, PhD, Chair of the AUA Renal Mass Guideline Panel and Vice Chairman of Urology at Cleveland Clinic. There are varied philosophies about management—often more related to the healthcare setting, region and surgeons’ training.
Dr. Campbell, colleague Christopher Weight, MD, and two other leaders in the field (and former fellows from Cleveland Clinic), Ithaar Derweesh, MD, and Robert Uzzo, MD, MBA, presented a course at the 2023 AUA Annual Meeting using a case-based approach to highlight the decision-making process and the updated guidelines.
The guideline states that radical nephrectomy should be considered whenever increased oncologic potential is suggested by tumor size, renal mass biopsy (RMB), and/or imaging features suggesting infiltrative or locally advanced features.
In this setting, radical nephrectomy is preferred if all of the following criteria are also met:
Advertisement
If these conditions are not met, a partial nephrectomy should be considered unless there are overriding concerns about the safety or oncologic efficacy of this procedure.
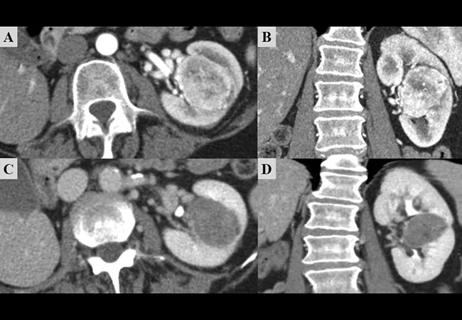
A 71-year-old male presented to Cleveland Clinic’s Department of Urology with a 4.9 cm hilar right renal mass. The tumor contour was somewhat irregular and the R.E.N.A.L. nephrometry score was 10. He had a history of coronary artery disease and a stent placed six years prior.
Based on imaging, the location of the tumor, near the hilum, would make a partial nephrectomy more technically challenging, and its irregular shape raised concerns for aggressive disease. The team considered the following:
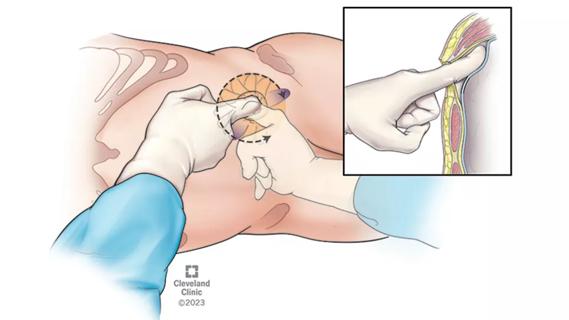
They ultimately elected to obtain a SRF to estimate the GFR of the contralateral kidney and an RMB to get more information about the tumor before making a decision.
“A partial nephrectomy would be a no-brainer if it was a solitary kidney. But it’s not and the contralateral kidney appears normal. Still, a partial nephrectomy is generally preferred because it preserves more function,” says Dr. Campbell. “But does it translate to better overall survival in this patient where the other kidney appears normal? Given the complexities with this case, we decided to obtain more information before surgery.”
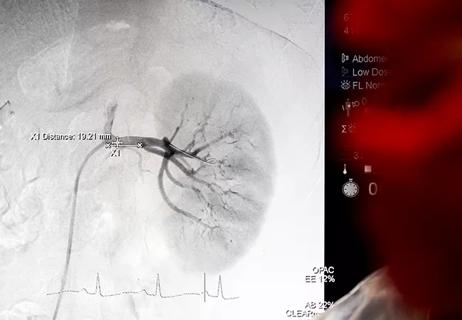
Using computerized software to measure parenchymal volume based on imaging — an analysis that has largely replaced nuclear renal scans at our center — the team identified a baseline GFR of 83 and an SRF of 53% and 47% on the left and right, respectively. The RMB indicated a clear cell, grade 3 malignancy, suggesting that the tumor biology might be on the more aggressive end of the spectrum.
Advertisement
Dr. Campbell uses a simple calculation to estimate the patient’s new baseline GFR following the radical nephrectomy: global GFR (83) x SRF contralateral x 1.25. The 1.25 coefficient is the average amount of renal functional compensation observed in adults after radical nephrectomy.
“Based on this, we proceeded with a radical nephrectomy, because our data suggested that the patient should end up with a GFR of 55, and he met all other criteria for radical nephrectomy,” he explains. Data show that reduced survival becomes a concern when a patient’s GFR is expected to fall below 45ml/min/1.73m2.
MIS radical nephrectomy confirmed that the malignancy was clear cell, pathological stage T3a (protruding into a branch vein), grade 4 with rhabdoid features, and all margins were negative. The patient’s post-operative GFR was 52, proximate to the team’s estimation of 55.
Overall, Dr. Campbell is pleased with their decision and the overall outcome. Four years later, the patient still shows no evidence of disease and maintains a GFR of > 50.
Though the tumor wasn’t large, it was — by all accounts — aggressive. The irregular contour on the imaging and RMB suggested increased oncologic potential. The SRF analysis revealed a normally functioning contralateral kidney, and an NBGFR estimation suggested it would maintain function following radical nephrectomy. In this case, Dr. Campbell explains, a partial nephrectomy could have put the patient at risk for more unfavorable outcomes.
“The goal is utilizing radical nephrectomy for patients who really need it, while reducing its overutilization. The AUA guideline — the only one that provides a granular description of criteria for radical nephrectomy — can be used to determine whether it is indeed the optimal treatment,” he concludes.
Advertisement
Advertisement
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

More than 30% of patients die when early dialysis is needed after surgery

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

New protocol reduces costs, increases patient and caregiver satisfaction
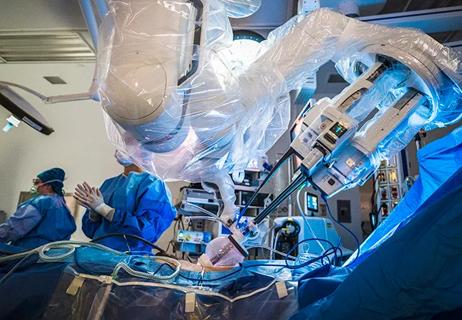
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients
General principles for use of the long-awaited new therapy approach
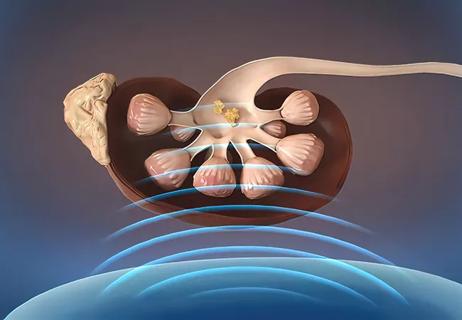
Cleveland Clinic is the first to investigate photonic nanoparticles as a potential kidney stone treatment
Management of high-risk RMSK in the pre-and current eras of neoadjuvant therapy