Technique offers many benefits for patients with very large prostates
Despite many factors in its favor, holmium laser enucleation of the prostate (HoLEP) to treat benign prostatic hyperplasia (BPH) has not achieved widespread popularity in the U.S.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Smita De, MD, PhD, a Cleveland Clinic urologist who performs HoLEP, advises urologists not be so quick to rule out this treatment option.
“In comparison with several other BPH procedures, the benefits of HoLEP include a shorter hospital stay, shorter time needed for catheterization and decreased bleeding risk,” Dr. De explains.
With HoLEP, the need for retreatment is much less of a problem than it is for patients who have had certain other noninvasive treatments. “The retreatment rate for HoLEP is typically less than 1-2%,” she notes. In comparison, the retreatment rate with TURP is between 6 and 18%.
Another advantage of HoLEP is that it can effectively treat very large prostates. “A lot of procedures, especially the newer ones like UroLift® and some other minimally invasive procedures, don’t necessarily work well on very large prostates,” Dr. De says.
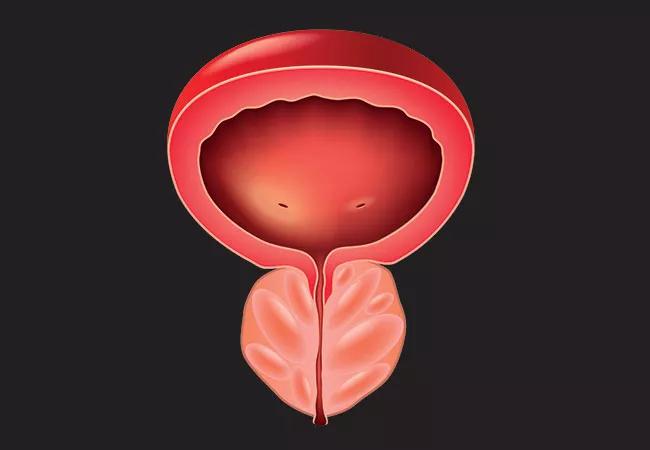
HoLEP, on the other hand, is a size-independent procedure. HoLEP approaches the task of treating BPH from a different direction than other noninvasive treatments. “Most other procedures for BPH work from the inside out,” she says. “They are carving out the middle of the prostate Roto-Rooter-style, like TURP, or ablating or lasering it from the inside.
“With HoLEP, we are working around the entire outside of the organ,” Dr. De says. “We are at the outer edges of the capsule trying to remove every bit. We are often able to get more tissue than those other procedures that work from the inside.”
Newness is not the issue, according to Dr. De. “HoLEP is not a new procedure; it’s been around since the 1990s. Dr. De suggests the following factors may be working against HoLEP:
Advertisement
HoLEP also may present some disadvantages. “HoLEP might be a longer procedure than some of the others available, so the patient must be under anesthesia longer,” Dr. De notes.
However, at the end of the day, Dr. De is a staunch proponent of HoLEP. At the same time, she says, “I don’t think that it’s a one-size-fits-all situation when it comes to choosing a procedure for treating BPH. Different procedures are appropriate in different situations, and for different patients.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key