Metabolic bone disease expert weighs evidence
Editor’s note: This article originally appeared in the Cleveland Clinic Journal of Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In short, no. Although calcium and vitamin D play an important role, they are not sufficient when used alone. Rather, they should be used in combination with an antiresportive agent such as estrogen, raloxifene, alendronate, risedronate or calcitonin.
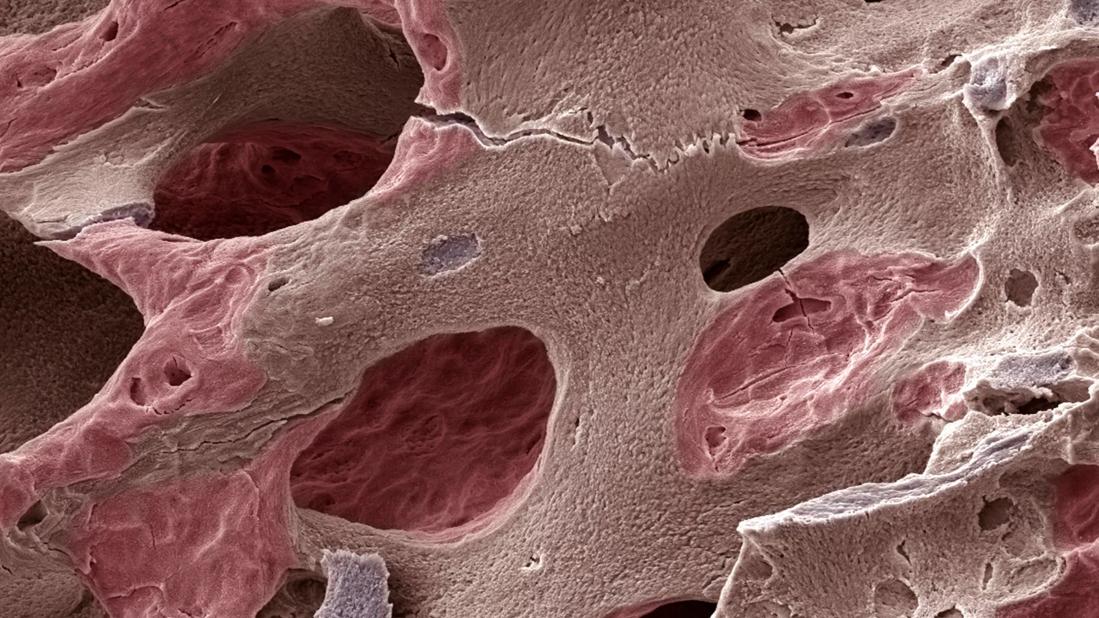
The World Health Organization has defined three levels of low bone mass; the definitions are based on T scores, which are standard deviation units below peak bone mass:
The National Osteoporosis Foundation recommends treatment with an antiresorptive agent in patients with a T score less than -2.0; patients with T scores less than -1.5 to -2.0 should also be treated if they have any of the following risk factors: family history of osteoporosis; previous fracture; current tobacco use; body weight less than 127 pounds. Many other factors such as steroid use are also important and houls be considered.
In almost all randomized controlled trials of antiresorptive agents, the control groups took calcium and vitamin D supplements. In these trials, patients who took alendronate, risedronate or raloxifene had significantly fewer fractures than those who took calcium and vitamin D alone. Thus, we conclude that supplements alone are not adequate.
Still, calcium and vitamin D are important in treating age-related bone loss, as they reduce the rate of bone loss and possibly reduce fracture risk.
Advertisement
To read the full in-depth answer to this question by Chad Deal, MD, Head of the Center for Osteoporosis and Metabolic Bone Disease, including an overview of studies of calcium and vitamin D, visit Cleveland Clinic Journal of Medicine. Dr. Deal reviews the use of biologics to treat metabolic bone disease here.
Advertisement
Advertisement

A conversation with Leonard Calabrese, DO

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.