Benefit/AFF risk ratio favors 3–5 years of treatment
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
JB, an 81-year-old, white female, presented with bilateral thigh pain of three months’ duration. She had osteoporosis with a lumbar spine T-score of –3.2 and had been on alendronate for 11 years. X-rays showed bilateral stress reactions in both femurs, on the lateral cortex, below the lesser trochanter consistent with atypical femur fractures (AFF). The left femur had an identified fracture line that did not extend to the endocortex, although she had both periosteal and endosteal elevation on x-ray. The patient was seen in orthopedics and intramedullary rodding was recommended, which the patient refused. She was treated with partial weight bearing and teriparatide for 24 months. The pain resolved in two months in the right thigh and 12 months in the left thigh.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/66bdfb4d-e9a2-4164-9e62-751dfaf9352e/21-RHE-2092912-AtypicalFemoralFracture-RApatients_CQD-inset1_453x619_jpg)
First reported in 2005, AFF were determined to be related to long-term therapy with bisphosphonates (BP). AFF have also been reported with denosumab and romosozumab therapy. AFF is extremely uncommon in the first three years of BP; however, the incidence increases with duration of treatment to 113 per 100,000 patient years after eight years.
In the FREEDOM trial open-label extension with denosumab, two participants developed AFF at three and seven years of treatment, which represents an incidence of 8 per 100,000 participant years.1 It is important to tell patients at high risk for fractures that the benefit/AFF risk ratio of 3–5 years of BP favors treatment: for every single AFF, approximately 1,200 osteoporotic fractures are prevented.2 Because the incidence of AFF increases with duration of therapy, the American Society for Bone and Mineral Research (ASBMR) developed guidelines for drug holidays from BP.3 For patients with no fractures and mild osteoporosis, ASBMR recommends 3–5 years of oral and three years for intravenous therapy (zoledronate).4 For patients with fractures and T-score of less than –2.5, the benefit/risk ratio favors up to 10 years of oral BP and six years of intravenous BP. With discontinuation of BP, the risk of AFF declines rapidly, and is 70% lower 12 months after discontinuation. The rapid decline is somewhat surprising since BP have a long residual half-life in bone, but also means that clinicians need to be alert to the possibility of AFF after discontinuation of BP.
Advertisement
Patients on long-term BP and denosumab therapy who present with thigh pain should have femur x-rays. Negative imaging with high suspicion for AFF warrants further imaging with MRI or CT. MRI scans show a bright signal on T2 images representing bone edema. ASBMR has also published a case definition of AFF, which is important since typical fractures of the femoral shaft occur in patients with osteoporosis.5
Providers should look at the femur shaft on DXA scans, as in our patient the scan periosteal elevation may be present and an early diagnostic sign. The fractures occur with no or minimal trauma and always originate on the lateral cortex, with periosteal elevation at the fracture site. They are below the lesser trochanter, and characteristically, when fractures occur they are not or minimally comminuted and transverse. Prodromal symptoms of thigh pain are usually present. Up to 25% of cases are bilateral. Groups at higher risk for AFF include patients on glucocorticoids and patients of Asian ancestry (in North America). In our patient, a DXA scan of the left femur in 2012 showed subtle periosteal elevation of the lateral cortex which was very prominent on the DXA in 2014.
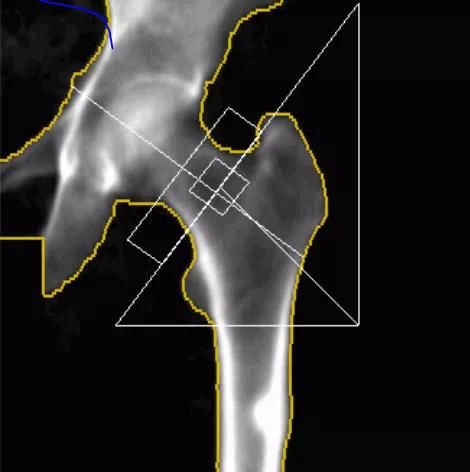
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7a74019e-aae4-4615-93f4-d3732d6bc8cc/21-RHE-2092912-AtypicalFemoralFracture-RApatients_CQD-inset2_470x472-1_jpg)
When an identified fracture line is present, treatment should include intramedullary nailing as many of the fractures will complete. BP or denosumab therapy should be discontinued. In a small series, more than 33% of patients with AFF completed their fracture without surgery, and another 33% had pain and delayed healing.6 There is a rationale for anabolic therapy since the mechanism of AFF is thought to be adynamic bone, with accumulation of microcracks that propagate to become a fracture. Numerous reports of PTH analogs have been published with mixed results. Teriparatide may accelerate fracture healing and reduce risk of non-union after treatment of intramedullary rods.
Advertisement
Our patient refused surgery and fortunately did not complete her fracture. In JB’s case, PTH analog therapy was associated with increased markers of bone formation, symptom improvement and rapid remodeling of the fracture site with resolution of the fracture line. At the end of teriparatide treatment, her lumbar spine T-score was –2.5. The use of antiresorptive agents would normally be recommended with a T-score of –2.5 and the knowledge that that bone loss will start after teriparatide discontinuation. This decision is always a difficult one when these agents were the initial cause for fracture. In this case, we started JB on raloxifene.
Dr. Deal is Head of the Center for Osteoporosis and Metabolic Bone Disease.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis