Puzzling constellation of findings lead to CT-guided bone biopsy
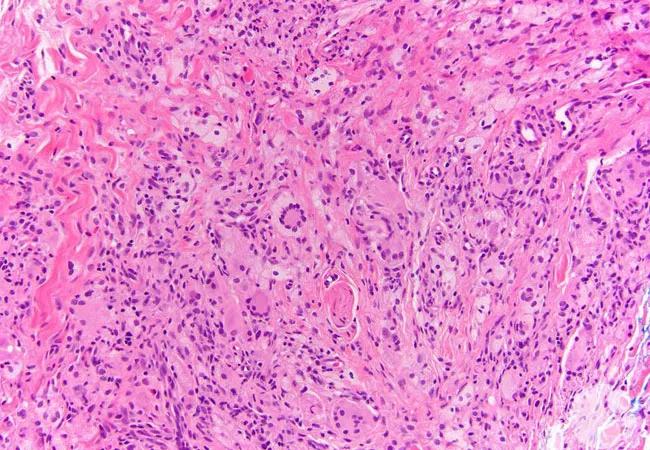
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/afcf1311-5c6d-4e7b-a6df-b83e30847f90/20-RHE-2006261-Deal_Keller_Erdheim-ChesterDisease-CQD-650x450-1_jpg)
20-RHE-2006261-Deal_Keller_Erdheim-ChesterDisease-CQD-650×450
By Sarah Keller, MD, MA, Leila Khan, MD, and Chad Deal, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 36 year-old-man presented to the metabolic bone clinic with two years of fatigue in the setting of high serum alkaline phosphatase (149 U/L , normal range 38 – 113 U/L). The patient reported pain in the bilateral thighs when doing physically intense labor; however, he denied additional symptoms. Past medical history included vitamin D deficiency, gastroesophageal reflux disease and depression. There was no history of a fragility fracture. Medications at the time of presentation included: vitamin D3 supplementation at a dose of 2,000 international units daily, omeprazole 20 mg daily and fluoxetine 20 mg daily.
Serum vitamin D 25-hydroxy was 26.7 mg/dL (normal range 31 – 80 ng/mL). Serum calcium and parathyroid hormone were within normal limits. Aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), and bilirubin were within normal limits. The bone fractionation of alkaline phosphatase was elevated at 28.6 uG/L (normal range 6.5 – 20.1 uG/L). A whole-body nuclear bone scan obtained at an outside facility and interpreted by a Cleveland Clinic radiologist demonstrated heterogenous and moderately intense uptake in the calvarium, the bilateral upper extremities (bilateral humeral diaphysis and bilateral radius) and bilateral lower extremities (distal femurs, proximal tibia and distal fibula). Uptake in the left femur was interpreted as having a “blade of glass” appearance, a classic finding in Paget disease. The impression of the bone scan was that findings could be consistent with the secondary phase of Paget disease; however, evaluation was limited as the study was obtained at another institution. Plain radiographs of the left lower extremity demonstrated patchy areas of sclerosis and lucencies in the distal femur and proximal tibia, corresponding to the regions of increased uptake on bone scan. A positron emission tomography and computed tomography scan (PET CT) obtained at an outside facility concluded that none of the sclerotic lesions demonstrated any fluorodeoxyglucose (FDG) avidity. Magnetic resonance imaging (MRI) of the bilateral lower extremities demonstrated large areas of heterogenous low T1 signal and increased T2 signal throughout the bilateral femurs, tibia, fibula and visualized pelvis/sacrum. MRI raised the question of a diffuse bone marrow infiltrative process.
Advertisement
The constellation of findings in this case was puzzling. While the elevated alkaline phosphatase and the findings on the bone density scan and radiographs raised the question of Paget disease, there were several aspects of this case that did not fit with this diagnosis. First, Paget disease is rarely diagnosed before the age of 40 with increasing incidence over the age of 60.1 Second, despite the “blade of grass finding,” the high intensity of uptake on the bone scan was more suggestive of that seen in metastatic disease or bone marrow reconversion and was not typical of Paget disease.1 The lucency and symmetry of lesions in the appendicular skeleton led to the following potential causes: medullary bone infarctions, malignancy, bone marrow reconstitution and Erdheim-Chester disease (ECD). Given the need for more information, the decision was made to pursue a CT-guided bone biopsy.
Bone biopsy of the femur demonstrated fibrohistiocytic proliferation of CD68 positive foamy histiocytes mixed with fibrosis and occasional lymphocytes. The pathologic diagnosis was ECD.
A malignancy of histiocytes from the monocyte-macrophage lineage, ECD is caused by mutations of BRAF and other signaling molecules in myeloid progenitor cells. While ECD is reported as a rare disease, the true incidence of ECD is not known, and it is thought that the disease incidence is under-represented in the literature.2 According to one systematic review of 259 patients with ECD, the long bones are almost always involved and the most common clinical manifestations included: skeletal involvement (26%), neurologic symptoms (23%), diabetes insipidus (22%), constitutional symptoms (20%), retroperitoneal involvement (14%), pulmonary symptoms (12%), cutaneous involvement (11%), cardiovascular manifestations (6%) and other pituitary involvement aside from diabetes insipidus (3%) .2
Advertisement
ECD is primarily treated by oncology and this patient was referred to oncology following bone biopsy for staging and chemotherapy.3 However, the complications that can arise in this disease and the myriad clinical manifestations require a team approach. In this case, ECD has been further complicated by the development of diabetes insipidus, for which the patient is being treated with desmopressin, as well as by primary hypogonadism, for which he will likely be treated with testosterone, highlighting the need for close follow-up with endocrinology.
This case underscores the need to maintain a high index of suspicion for diseases that can mimic rheumatic processes as well as the essential nature of the multidisciplinary approach to the evaluation and management of patients with complex presentations of rare diseases.
Please note: The image above was originally published in ASH Image Bank. Morgan E, Patel S. Erdheim-Chester disease. ASH Image Bank. 2018;00061844. ©The American Society of Hematology.
Advertisement
Dr. Keller (@skeller1016) is Associate Staff in the Department of Rheumatologic and Immunologic Diseases. Dr. Khan is Staff in the Department of Endocrinology, Diabetes and Metabolism. Dr. Deal (@CLDeal) is Head of the Center for Osteoporosis and Metabolic Bone Disease.
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being