Advertisement
Study presented at ASTRO 2021 shows promise in patients treated with stereotactic radiosurgery

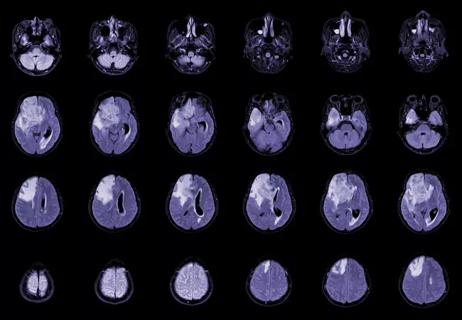
A prospective pilot study conducted in 16 patients with brain metastases found that 18F fluciclovine PET CT demonstrated promising utility in distinguishing radiation necrosis from tumor progression among patients treated with stereotactic radiosurgery (SRS). Early findings from this study were presented at the American Society for Radiation Oncology (ASTRO) 2021 Annual Meeting held in Chicago on October 24-27, 2021 by Martin Tom, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is the first de facto prospective study that is really using 18F fluciclovine PET CT to try to distinguish between the two,” says Cleveland Clinic radiation oncologist Samuel T. Chao, MD, corresponding author of the study. “Obviously, it does require further studies, such as larger multi-institutional-type studies like PURSUE and REVELATE, but it certainly did prove to us that this particular drug has diagnostic utility.”
In explaining the rationale behind this work, Dr. Chao notes that radiation necrosis is a fairly common complication of SRS, occurring in approximately 5-10% of patients; however, differentiating between radiation necrosis and tumor progression remains a challenge in the clinical setting. “The problem is that we don’t know with 100% certainty if the tumor is coming back or if the patient has developed radiation necrosis,” he says. “Both on MRI and both problems are associated with swelling, so we have to use the different tools that we have in our tool belt to try to pinpoint the culprit.”
According to Dr. Chao, one of the tools used in this situation is cerebral blood volume, which assesses blood flow in the brain. Other potentially useful techniques include MR spectroscopy, which has an accuracy above 80%; fluorodeoxyglucose (FDG)-PET, which has varying levels of accuracy due to the brain taking up a lot of glucose; and amino acid-PET. However, Dr. Chao notes that most of the mentioned techniques are not discriminative enough. While amino acid-PET is fairly accurate in distinguishing between radiation necrosis and tumor progression, its limitations include the need to synthesize or purchase 18F-labeled, which are not easily available.
Advertisement
“The good thing is that fluciclovine has been around more recently and has been used to diagnose metastatic prostate cancer,” he says. “It’s FDA approved specifically for that indication, and it is easily obtainable.”
The purpose of this latest study was to assess whether fluciclovine can be used to specifically distinguish between tumor recurrence and radiation necrosis. The study enrolled a total of 16 patients treated for brain metastases at Cleveland Clinic between July 2019 and November 2020. Of 16 enrolled patients, 15 were evaluable with a total of 20 lesions. In nine brain lesions the primary histology was non-small cell lung cancer, breast cancer was the primary tumor in seven lesions (35%), melanoma in three (15%), and endometrial cancer in one (5%). For 16 lesions the final diagnosis was tumor necrosis, and for the remaining four it was tumor progression.
“When we used fluciclovine, our ability to identify tumor progression was very good — it was 100%,” says Dr. Chao. “Our ability to rule out tumor progression may be less accurate, but keep in mind that this is just an early study with a limited number of patients. We’re hoping to refine some of that with future studies.”
Advertisement
The authors looked as SUVmax, SUVmean and SUVpeak, the parameters that indicate the level of fluciclovine uptake, and all seemed to be fairly effective in distinguishing between radiation necrosis and tumor progression. Normalizing it compared to normal, SUVpeak/normal seemed to be the best to differentiate between the two pathologies. “We also looked at what we call visual inspection,” adds Dr. Chao. “Rather than rely on all these specific values, the physician would just look at the scan and say the problem is tumor recurrence or radiation necrosis. And depending on how they looked at it, two out of the three nuclear medicine docs were able to interpret that pretty accurately.” These nuclear medicine physicians were not specifically trained to interpret these scans, so training would likely improve their accuracy with simple inspection. This would make interpretation facile.
Dr. Chao acknowledges that the weakness of the study is its small size and the fact that only a had biopsies, but he notes that the findings have nevertheless proven invaluable in informing follow-up research. A larger study, RELEVATE, sponsored by fluciclovine’s manufacturer, Blue Earth Diagnostics, is already recruiting patients. The purpose of this trial is to examine the utility of fluciclovine in real-world clinical situations, with most patients undergoing clinical follow-up after undergoing imaging. This study is important, Dr. Chao explains, because the course of treatment for tumor recurrence vs radiation necrosis is very different.
“If it’s tumor recurrence, we may consider surgery, more radiation or systemic therapies that could target that particular tumor,” he says. “But if the pathology is more consistent with radiation necrosis, we may sometimes consider surgery, laser ablation or even Trental/Vitamin E, bevacizumab or hyperbaric oxygen.”
Also, the earlier we treat these patients, whether for tumor recurrence or radiation necrosis, it is likely that the outcomes will be better in terms of preventing further neurological issues and decline,” he concludes.
Advertisement
Advertisement

Key research findings to watch

Timing and type of side effects differ greatly from chemotherapy

Dedicated multidisciplinary teams support 84 ultra-rare cancers
New research from Cleveland Clinic helps explain why these tumors are so refractory to treatment, and suggests new therapeutic avenues
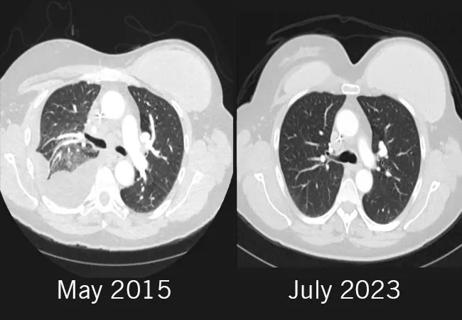
Combination of olaparib and carboplatin results in complete durable response for a patient with BRCA2 and “BRCAness” mutations

Early communication between oncologists and ophthalmologist warranted
Case-based course delves into latest treatment approaches

Long-term relationship building and engagement key to gaining community trust