A case study from Rula Hajj-Ali, MD
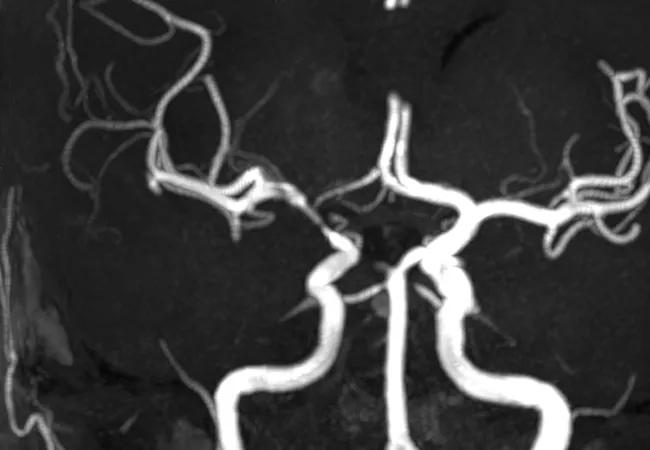
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c66b8908-9c2e-49fa-a1a4-62d9c2214c04/17-RHE-1241-Hajj-Ali-Hero-Image-650x450pxl_jpg)
Imaging of vessels in CNS vasculitis
A 56-year old presented with manic symptoms and encephalopathy. Following work-ups for infection and malignancy, which included a brain biopsy, she was diagnosed and treated for primary angiitis of the central nervous system (PACNS) at an outside hospital. However, she had a transient response and then became progressively worse and was transferred to our hospital.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In this video, vasculitis specialist Rula Hajj-Ali, MD, presents the complex case that seemed refractive to treatment. Is it really central nervous system vasculitis (CNS-V)?
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/SMrSZ_yDHNs?feature=oembed)
What Would You Do? Is It CNS Vasculitis?
Arriving at a diagnosis of CNS-V is fraught with challenges. Clinical presentation can be quite variable, and there is no classic presentation. Further complicating matters, the condition has several mimics, brain tissue is inaccessible and there is no disease-specific test. However, advances in neuroimaging and next-generation sequencing — along with the involvement of a multidisciplinary clinical team — have added formidably to our knowledge of CNS-V.
Regardless of the scenario, we take a systematic approach to the work-up of any patient suspected to have CNS-V. This approach includes a general history and physical exam, with a thorough review of symptoms associated with systemic autoimmune disease (e.g., fever, rashes, sinus disease, sicca, joint pains, cough, peripheral neuropathy, oro-genital ulcers, inflammatory eye disease, deep venous thrombosis or recurrent miscarriages). Clinicians should look for infectious and/or malignant conditions that might be associated with many of these nonspecific symptoms, especially fever, malaise, joint pains and weight loss. Other important aspects when interviewing patients include eliciting travel history, work hazards, chronic exposure to recreational drugs and family history of neurologic events; this information can unravel rare conditions.
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being