Knowing the affected organs and vessels can help in identifying cause
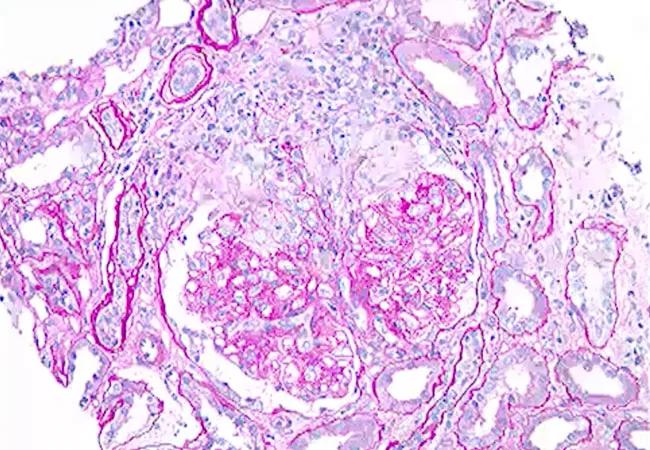
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d12df1c7-4a5b-4397-b96b-2cde59db9a71/21-RHE-2528446-Monitoring-patients-ANCA-associated-vasculitis-CQD_650x450_jpg)
21-RHE-2528446-Monitoring-patients-ANCA-associated-vasculitis-CQD_650x450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Chapel Hill Consensus Conference nomenclature divided vasculitides based on several combinations of features. One of these divisions is primary versus secondary, based on whether the vasculitis is associated with or caused by a systemic disease or drug.1 Secondary vasculitides can be associated with and/or caused by infections such as hepatitis B, causing cryoglobulinemic vasculitis; underlying autoimmune disorders, such as rheumatoid vasculitis; and certain drugs, such as cocaine, causing anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV); and malignancies.
The clinical presentation of secondary vasculitides may share symptoms as well as laboratory, radiographic and pathological findings with primary vasculitides. Identifying the potential cause, such as a drug or underlying autoimmune disorder, is extremely important for management and prognosis. In A Spotlight on Drug-Induced Vasculitis,2 we highlighted common drugs known to cause vasculitis based on the size of the affected vessels and involved organs. We further discussed clinical phenotypes, risk factors, treatments and outcomes. What follows is a more abbreviated look at drug-induced vasculitis (DIV).
Small vessel vasculitis predominantly affects intraparenchymal arteries, arterioles, capillaries and venules, which may or may not involve immune complex deposition in vessel walls.
• Drug-Induced ANCA-Associated Vasculitis: Hydralazine, propylthiouracil and cocaine are considered the most common drugs to be associated with AAV. The clinical presentation varies from non-severe vasculitis to potentially life-threatening multi-organ involvement. Clinical suspicion should be high when leukopenia, thrombocytopenia, dual-positive ANCA patterns, and overlapping serologies between AAV and systemic lupus erythematous are present, which all are uncommon in primary AAV.
Advertisement
• Drug-Induced Small Vessel Vasculitis with Immune Complex Deposits: Immunoglobin A vasculitis is an immune complex-mediated, small vessel vasculitis with IgA1-dominant immune deposits. It has been associated with infections, malignancies and autoimmune diseases. It can be caused by exposure to medications including quinolones and clarithromycin, furosemide, nonsteroidal anti-inflammatory drugs (NSAIDs), tumor necrosis factor-α (TNF-α) inhibitors, and many other drugs.
Polyarteritis nodosa (PAN) is the most common primary medium vessel vasculitis. Historically, minocycline is reported to be the drug most frequently drug associated with PAN. Most cases reported to date are isolated cutaneous PAN followed by systemic vasculitis with multiple organ involvement such as nerves, muscles or kidneys. In contrast to primary PAN, patients with minocycline-induced medium vessel vasculitis are commonly found to have positive ANCA antibodies. Prognosis is favorable, as complete resolution has been reported in most cases of minocycline-induced PAN.
Large vessel vasculitis affects the aorta and its major branches. The most common forms are giant cell arteritis, Takayasu’s arteritis, and isolated aortitis. Aortitis and large vessel vasculitis are rarely reported complications of granulocyte colony-stimulating factor and other cancer-related therapies, including gemcitabine and immune checkpoint inhibitors (ICIs). Most of the reported cases manifested as fever of unknown origin, unexplained weight loss and lethargy in addition to localized symptoms based on the vascular territory involved. Vessel wall thickening was the most reported finding on different imaging modalities.
Advertisement
Drug-Induced Single Organ Vasculitis involves:
• Drug-Induced Cutaneous Vasculitis presenting as ulceration, digital ischemia or purpuric rash, which may be triggered by antibiotics, NSAIDs, TNF-α inhibitors and various other medications.
• Drug-Induced Cerebral Vasculitis presenting as new onset headache, focal neurological symptoms, seizure or change in mental status, which is typically associated with amphetamines and cocaine abuse. • Drug-induced Vasculitic Neuropathies presenting as mononeuropathy, mononeuritis multiplex or sensorimotor polyneuropathy. Drugs implicated as triggers of non-systemic vasculitic neuropathies, which are quite rare, are TNF-α inhibitors, ICIs (nivolumab, pembrolizumab), and minocycline.
A high index of suspicion for DIV is required for prompt diagnosis and treatment, which begins with removing the inciting drug. Administering glucocorticosteroids is recommended in nonsevere cases. Addition of a second agent may be necessary in severe presentations with organ or life-threatening vasculitis.
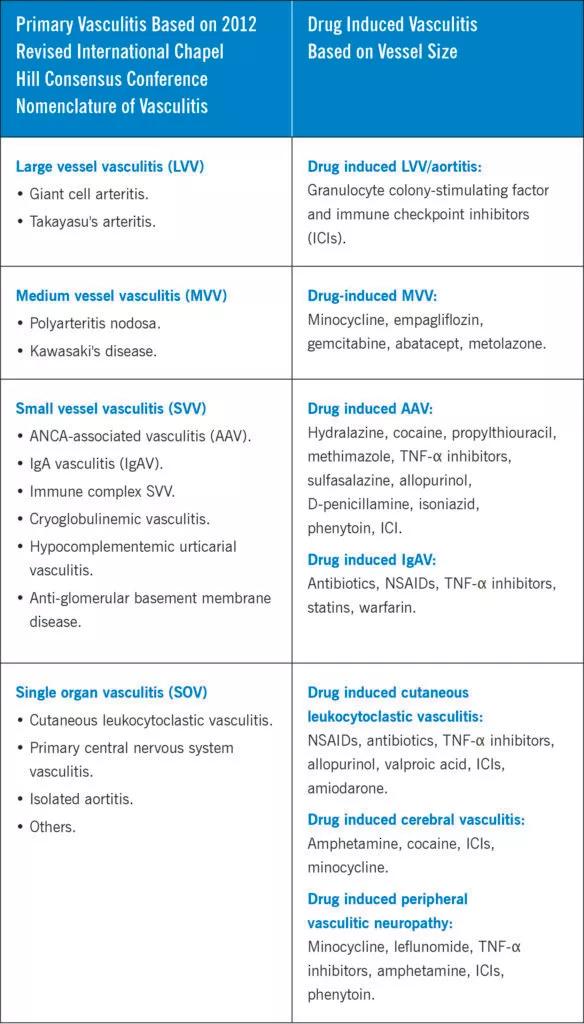
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f659e7db-1873-4a02-84d9-11b5af5260d0/23-RHE-3662511-CQD-Inset-584x1024_jpg)
References
1. Jennette JC, Falk RJ, Bacon PA, et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
2. Yaseen K, Nevares A, Tamaki H. A spotlight on drug-induced Vasculitis. Curr Rheumatol Rep. 2022
Nov;24(11):323-336.
Advertisement
Advertisement
Evidence-based therapies, monitoring, prevention and more
Holistic approach is necessary to ensure a correct diagnosis
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
Unraveling the TNFA receptor 2/dendritic cell axis
Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis
Genetic testing at Cleveland Clinic provided patient with an updated diagnosis
Combining quantitative vessel wall MRI metrics, CSF abnormalities and neurologic symptoms can be highly predictive
From dryness to diagnosis