Relapses are frequent even with long periods of remission
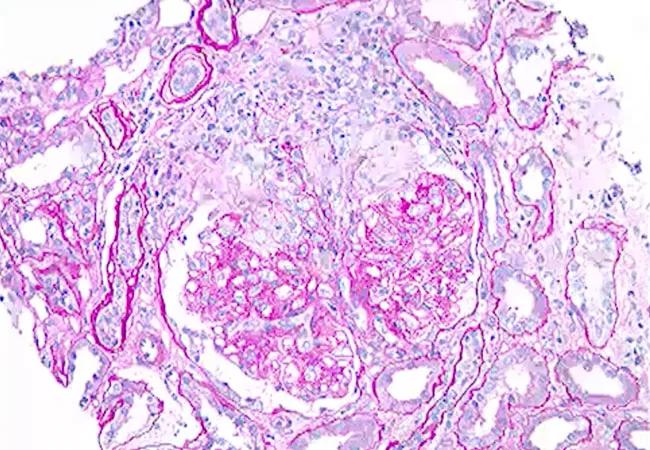
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d12df1c7-4a5b-4397-b96b-2cde59db9a71/21-RHE-2528446-Monitoring-patients-ANCA-associated-vasculitis-CQD_650x450_jpg)
21-RHE-2528446-Monitoring-patients-ANCA-associated-vasculitis-CQD_650x450
A 42-year-old man presented with a history of recurrent sinusitis and nasal bleeding with a large amount of crusting. He also experienced bilateral eye watering, light sensitivity and redness as well as migratory joint pain. Computed tomography (CT) of his sinuses showed pansinusitis, while CT chest was normal. An ophthalmologic exam showed scleritis. Laboratory test results, including erythrocyte sedimentation rate and proteinase 3 antineutrophil cytoplasmic antibodies (ANCA), were consistent with a diagnosis of granulomatosis with polyangiitis (GPA).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
GPA is an antineutrophil cytoplasmic autoantibody-associated vasculitide disorder, characterized by systemic autoimmune small-vessel vasculitis. It can affect the lungs, kidneys, airway and sinonasal regions. Despite many advances in treatment, 50 to 70 percent of patients experience relapses after remission induction.
The patient received induction therapy of rituximab and prednisone. Remission was achieved, and he was on maintenance therapy with daily azathioprine for two years with the following year off therapy.
His symptoms and labs were monitored monthly, and a full three years later, testing revealed elevated creatinine and microhematuria and red blood cell casts in the urine. He remained asymptomatic, but a kidney biopsy showed pauci-immune necrotizing crescentic glomerulonephritis, a clear indicator of relapse with renal involvement. He again received induction therapy with tituximab and prednisone. Remission was achieved, and he was then kept on maintenance therapy with rituximab.
Learn more below from Alexandra Villa-Forte, MD, MPH, staff in the Center for Vasculitis Care and Research in Cleveland Clinic’s Department of Rheumatic and Immunologic Diseases.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/3M6uvjYQHN4?feature=oembed)
Monitoring Patients With ANCA-Associated Vasculitis
“This case illustrates the importance of monitoring patients with ANCA-associated vasculitis,” says Dr. Villa-Forte. “Relapses are very frequent in GPA, especially during times when patients are off therapy. Relapses may be asymptomatic, and therefore long-term monitoring of patients with GPA is critical for early diagnosis and treatment.”
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being