Subtle information gleaned from clinical examinations prompted concern
A 57-year-old male presented with right-sided facial numbness, dizziness and otalgia that he had been experiencing for the past five months. He reported a rather insidious onset of his symptoms with progression over time. He had no significant previous medical history.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
He was assessed by neurology nurse practitioner (NP), Sarah Hrestak, APRN, CNPS for the above complaints. The patient had subjective right-sided facial/tongue numbness and decreased taste. He also complained of daily vertigo upon waking up that could be exacerbated by the extension of the neck. In addition, the patient noted new daily chronic headaches without red-flag symptoms.
Objectively, there was decreased sensation of the right trigeminal nerve V1 through V3 and positive sustained nystagmus with left lateral gaze. There was a decreased left-arm swing, and he fell to the right while walking. Hrestak was initially concerned for a potential demyelinating process and ordered the appropriate diagnostic workup.
An audiological evaluation and vestibular testing were completed the following day by Evalena Behr, AuD. His initial presentation had improved after a self-administered Epley maneuver but persisted particularly with swift lateral head movements (right or left). He also reported reduced word understanding abilities and hyperacusis (sensitivity to sounds) in his right ear.
The audiological evaluation revealed bilateral high-frequency sensorineural hearing loss worse on the right side (Figure 1). His word recognition scores (WRS) were 80% for the right ear and 100% on the left.
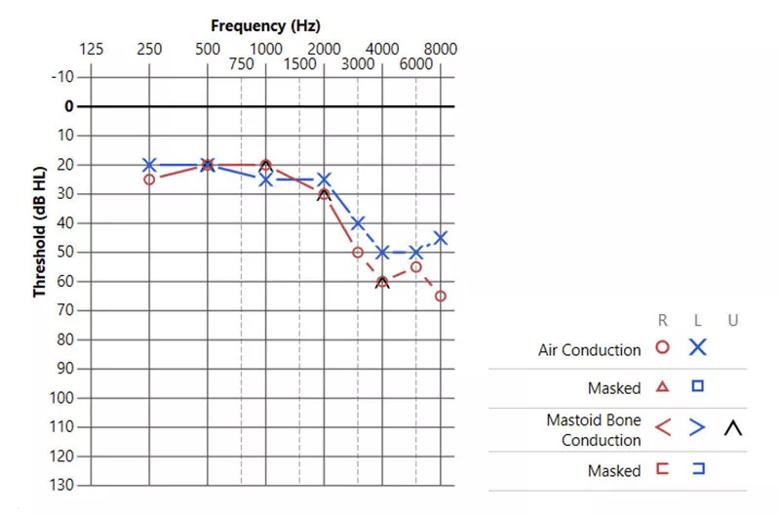
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0006cbc2-4988-4b97-8023-eabd75a4cd4c/graph-audiology-test)
Figure 1. The y-axis represents intensity level of sound measured in decibels (dB HL). Soft sounds are found at the top of the graph (-10 dB HL), with louder sounds at the bottom (130 dB HL). The x-axis represents the frequencies of sound measured in hertz (Hz). Low frequency sound is near the left portion of the graph with the highest frequencies at the right. The red circles represent right ear hearing, while the blue “Xs” represent the left ear.
The vestibular test battery (VTB) revealed uncompensated right-sided vestibular hypofunction. However, during testing, bedside examination revealed lagophthalmos (incomplete closure of the eyelid) of the right eye, along with reduced facial function in all divisions on the right side. Although portions of the objective testing could be consistent with a peripheral vestibular pattern, the patient’s right-sided facial paresthesia and weakness, and observed ocular abnormalities — especially the presence of nystagmus despite fixation — raised suspicion for central vestibular involvement.
Advertisement
Neurotologist and Section Head of Otology and Neurotology, Marc Bassim, MD, saw the patient shortly thereafter. The examination of the patient’s face revealed a Grade II facial nerve function on the House-Brackman scale (on a scale of Grades I-VI, with Grade I being normal).
Considering the overall clinical presentation and results from audiological and vestibular testing, an expedited MRI of the internal auditory canals was completed. The neuroimaging confirmed previous providers’ concerns, noting “abnormal signal of the right dorsolateral pontomedullary junction in the region of medial and inferior vestibular nuclei, posterior cochlear nucleus, nucleus of the tractus solitarius and inferior cerebellar peduncle, suggestive of demyelination (Figure 2).
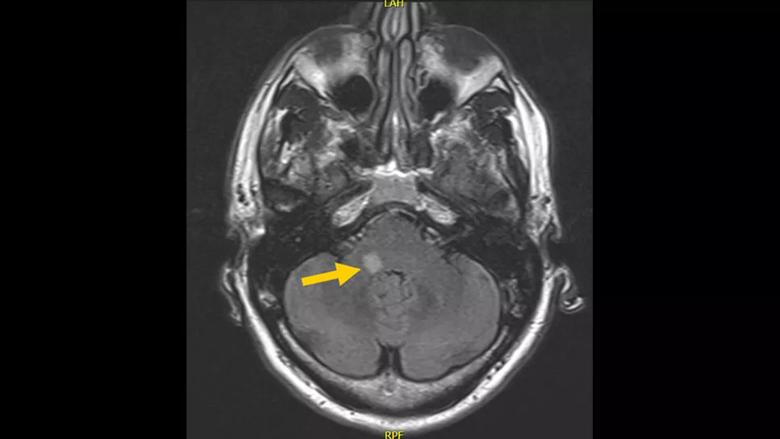
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/db0b64ea-e9b6-4e3c-b62f-98aac1963f36/mri-image-of-skull)
Figure 2. The demyelination lesion described above is illustrated on this MRI section in the right pontomedullary junction.
Dr. Bassim and Hrestak discussed the results and the provider’s concerns about a central process to account for the patient’s vertigo. Hrestak helped facilitate a timely referral to the Mellen Center for Multiple Sclerosis for further evaluation of possible demyelinating disease.
The patient was evaluated by neurologist, Kedar Mahajan, MD, PhD who confirmed the diagnosis of clinically isolated syndrome (right dorsolateral pontomedullary junction) with lower risk for conversion to clinically definite multiple sclerosis based on prognostic criteria (absence of other T2 lesions and negative oligoclonal bands).
Based on the above findings, the patient was started on high-dose prednisone, initially at 1250mg per day for five days. He was also started on vestibular rehabilitation for his dizziness.
Advertisement
At his latest follow-up appointment, he had complete resolution of his dizziness, facial weakness and hypesthesia. He will be monitored on a regular basis both clinically and with imaging.
This case report highlights the value of prompt multidisciplinary collaboration to establish a diagnosis in patients presenting with atypical cases of vertigo. Though rare, there are documented cases of a clinically isolated syndrome resulting from a demyelinating lesion that initially manifests with otologic symptoms (Veros et al., Am. J. Otolaryngol. 2014;35[5]:683-686). The interaction between specialists influenced the course for this patient, ultimately leading to a critical and timely diagnosis.
The importance of clinical information derived from the neurotological and audiological examinations is also exemplified. Although the findings of the vestibular assessment closely resembled a peripheral vestibular lesion, subtle findings prompted concerns about central vestibular involvement. This case also brings awareness of atypical patients with vertigo and multilevel neuropathy and the importance of thorough and prompt evaluations.
Advertisement
Advertisement
Today’s research helps illuminate tomorrow’s needs
Input from these central stakeholders is leading us to design for healing and hope
Novel ‘assessment center’ will be a partner in care by serving as an engine of structured data collection
What it’s like working in neurology critical care and what to consider before entering the specialty
How a new clinic is helping to streamline evaluations for patients
Case series links catastrophic outcomes to therapy initiation within 48 hours post-procedure
Scientific program chair reflects on what may resonate longest from this year’s neurosurgery conference
Neurology is especially well positioned for opportunities to enhance clinical care and medical training