Redundant leads complicate treatment of device infections, study shows
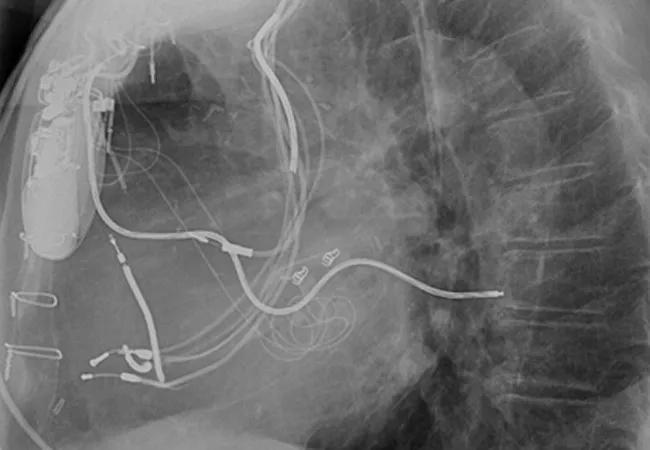
As the popularity of cardiac implantable electronic devices (CIEDs) explodes, the number of infections linked to abandoned leads is growing exponentially. These unwanted leads complicate the management of CIED infections and result in worse outcomes, including death, Cleveland Clinic electrophysiologists have found.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This finding, as published online by JACC: Clinical Electrophysiology on Sept. 7, was based on a study from a prospective registry of consecutive patients undergoing transvenous lead extraction of infected CIEDs at Cleveland Clinic between August 1996 and September 2012.
The 1,386 patients with infected devices were divided into two groups: those with (23.3 percent) and those without (76.7 percent) previously abandoned leads. Failure to achieve the study’s primary end point — successful removal of the device and all lead material from the vascular space without a major complication — was significantly more common in patients with abandoned leads (13.0 percent) than in patients without abandoned leads (3.7 percent) (P < .0001).
Lead author Oussama Wazni, MD, says the study was undertaken due to frustration with the high rate of unwanted leads left in patients.
“It’s a growing problem for us, because we deal with the ones that get infected,” he says. “After about a year, the leads get attached to the veins or atrium and develop fibrosis. It becomes difficult to release them from their binding sites without causing damage.”
More than 300,000 patients receive CIEDs in the U.S. every year. Many of these patients will require access to the device pocket for a system change, revision or upgrade, opening the door to infection. Such infections carry a mortality risk as high as 66 percent. Even with total extraction and antibiotic therapy, the risk may remain as high as 18 percent.
Risk is elevated when a patient with infection has an abandoned lead.
Advertisement
“It’s a common practice that postpones risk now but gambles on the patient’s future,” says Dr. Wazni. “Some physicians may ask why they should expose a patient to risk and complications now, when it’s easier to simply add a lead. But such physicians are not taking into consideration the potential need for the lead to be removed at a future date when there is no choice due to infection.”
Although most electrophysiologists receive training in lead extraction, many do not perform the difficult procedure often enough to gain a level of comfort with it. Others may be comfortable doing uncomplicated extractions but hesitate when the lead is damaged. Such patients should be referred to a center that specializes in lead extraction.
There are times when lead extraction is not desirable. Anticoagulant use is a contraindication, as is the presence of a serious comorbidity — for example, a low platelet count or liver disease. Frailty with advanced age may also be a consideration.
“Occasionally, we’ll have a very elderly patient who needs a new lead,” Dr. Wazni explains. “In such a case, we would not extract the old one, because the procedure may be too difficult for the patient to tolerate. But most times, we extract leads that would otherwise become redundant.”
Although the decision to abandon or remove superfluous leads needs to be made on a case-by-case basis, there is growing recognition that abandoning leads complicates the management of CIED infections and results in worse clinical outcomes. The Heart Rhythm Society is in the process of drafting guidelines designed to clarify when leads should be removed.
Advertisement
“It’s not an easy decision,” says Dr. Wazni. “Lead extraction is a complex intervention with inherent risks that need to be weighed against the risks of lead abandonment.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more