Follow-up study confirms safety and tolerability of new treatment protocol
An ongoing phase 2 trial conducted by a team of Cleveland Clinic investigators has found that the monoclonal antibody CAEL-101, when used in combination with anti-plasma cell dyscrasia (anti-PCD) therapy, may prevent downstream complications in patients with cardiac amyloid light-chain (AL) amyloidosis. Findings from the one-year follow-up study were presented at the 2021 American Society of Hematology Annual Meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“If approved, CAEL-101 is going to change the lives of thousands of patients with AL amyloidosis,” says hematologic oncologist Jason Valent, MD, who led the study in Taussig Cancer Institute.
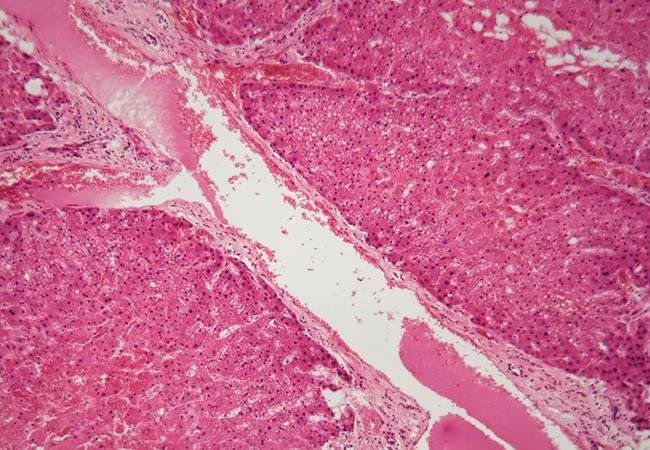
AL amyloidosis is an incurable plasma cell disorder responsible for approximately 4,000 new cases in the US per year. It is characterized by the deposition of amyloid fibrils, produced by defective plasma cells, in tissues and organs. Left untreated, the accumulation of these amyloid fibrils eventually leads to organ dysfunction and death.
“Standard treatment for AL amyloidosis entails a combination of daratumumab, bortezomib, cyclophosphamide and dexamethasone,” says Dr. Valent. “In most cases, these drugs are effective at reducing or shutting off the production of the abnormal protein. However, the treatment does nothing to help remove the abnormal antibody that’s already deposited in the vital organs.”
To date, there are no approved therapies capable of removing the amyloid fibril deposits — which is a major unmet need. “The biggest problem that we have is that a lot of the patients we see have severe end-organ damage — life-threatening heart failure or kidney problems — and there’s only so much that we can do to halt this progression with the currently available treatments. A drug like CAEL-101, which has the potential to reverse end-organ damage early in the course of therapy, is critically important,” says Dr. Valent.
CAEL-101 is a monoclonal antibody that acts by binding to amyloid light-chain fibrils and promoting their clearance from affected tissues.
Advertisement
“When the [CAEL-101] antibody sticks to the fibril, it triggers the immune system to come in and clear out the amyloid fibril,” Dr. Valent explains. An earlier phase 1 study of 500 mg/m2 CAEL-101 alone showed the drug held promise in previously treated patients with AL amyloidosis who had persistent organ dysfunction.
The current study was designed to assess whether CAEL-101 (in doses up to 1,000 mg/m2), when used in combination with anti-PCD therapy, is well tolerated and appropriate for use in a phase 3 trial. In part B of the study, daratumumab was added to the treatment regimen. The 12-month trial enrolled 25 adult patients with confirmed AL amyloidosis: 8.0% had Mayo stage I, 76.0% had stage II and 16.0% had stage IIIa disease. Study subjects were required to have measurable hematologic disease and at least a six-month life expectancy. Of those 25, 19 (76%) had cardiac involvement, eight (32%) had renal involvement and 20 (80%) had received prior anti-PCD therapy.
A total of 24 patients experienced some type of adverse event, but only six (24%) of those events were believed to be treatment related. The most common adverse events included nausea (36% of patients); constipation (32%); and diarrhea, fatigue or rash (28% each). Almost one-third (32%) of study participants experienced at least one grade 3 or higher adverse event, while 28% reported at least one serious complication.
“The overwhelming majority of patients who had kidney damage associated with amyloid had improvement in their proteinuria,” notes Dr. Valent. 24-hour urine protein is the lab test used by the consensus criteria to assess patient response. Eight of the nine patients with kidney involvement showed improvement in their proteinuria by greater than 30%, which is the cutoff. “All but two of the patients experienced an improvement by 70% or more,” he says.
Advertisement
“So, overall, a majority of patients with kidney involvement had an organ response, and 90% of the patients with heart involvement were either stable or responded,” Dr. Valent adds. “This is spectacular, in my mind. Although the drug certainly has good activity, it is now left to the ongoing phase 3 trials (one for Mayo stage IIIa and one for Mayo stage IIIb patients) to confirm the value of adding CAEL-101 to the standard chemotherapy regimen for the treatment of AL amyloidosis. We are participating in these international phase 3 trials and hope to complete enrollment by the end of 2022.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors