But such EEG findings should not preclude tapering of antiseizure medications
Most pediatric patients who are seizure-free after successful disconnective hemispherectomy continue to have abnormalities evident by electroencephalography (EEG) in the disconnected hemisphere. Nevertheless, many of these patients can be weaned off antiseizure medications (ASMs) with no recurrence of seizures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So reported researchers from Cleveland Clinic’s Charles Shor Epilepsy Center in a Dec. 5 platform presentation at the 2021 annual meeting of the American Epilepsy Society. The findings are from a series of 50 consecutive pediatric patients who became seizure-free following hemispherectomy.
“We want to raise awareness that young patients who are seizure-free after disconnective hemispherectomy may have EEG findings of epileptiform activity — and even subclinical seizures — in the disconnected hemisphere, but that this need not consign these patients to a lifetime of taking antiseizure medications,” says the study’s senior author, Ahsan N.V. Moosa, MD, a Cleveland Clinic pediatric epileptologist.
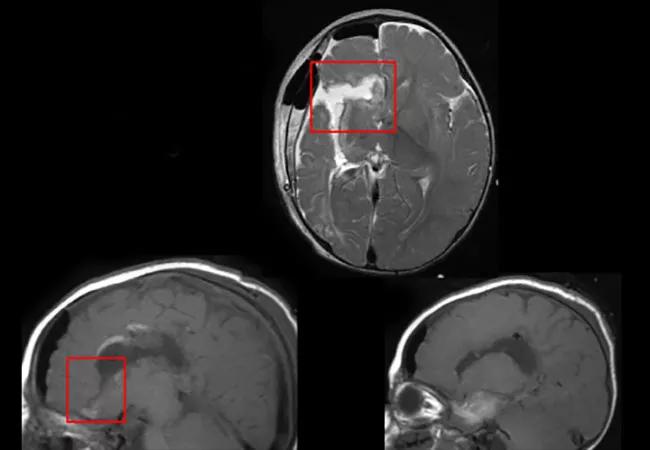
Disconnective hemispherectomy is an important option for selected patients with drug-resistant epilepsy. Cleveland Clinic’s experience from 170 patients who underwent the surgery between 1997 and 2009 resulted in about two-thirds being seizure-free after hemispheric surgery (Neurology. 2013;80:253-260).
However, a wide spectrum of abnormalities in the disconnected hemisphere may be seen on EEG after the operation. Although EEG abnormalities usually help determine whether a patient should be weaned off ASMs following surgery, the nature of these abnormalities and how they correlate with clinical outcomes have not previously been well characterized in the setting of disconnective hemispherectomy.
The current study analyzed 50 consecutive pediatric patients from Cleveland Clinic’s Epilepsy Surgery Outcome Database who were seizure-free at last follow-up after hemispherectomy. Mean age at surgery was 7.5 years (median, 6 years; range, 8 months to 21 years), and patients were evenly divided by sex (52% male/48% female).
Advertisement
Right hemispherectomy was performed in 23 patients (46%). Most underwent disconnective hemispherectomy (n = 47; 94%), with the rest having a modified anatomical hemispherectomy. Mean follow-up was 3.8 years (median, 3 years).
The most common causes of epilepsy were gliosis and encephalomalacia of various causes (including perinatal stroke), found in 35 patients (70%). Other causes were malformation of cortical development (n = 7), Rasmussen encephalitis (n = 6) and Sturge-Weber syndrome (n = 2). Thirty patients (60%) had a single seizure type; the rest had more than one.
Preoperative EEGs had features of epileptic encephalopathy in 12 patients (24%), consisting of hypsarrhythmia (n = 5), slow spike-and-wave complexes (n = 4) and continuous spike-waves during sleep (n = 3).
Postoperatively, EEGs of all patients exhibited slowing and attenuation of physiological rhythms in the operated hemisphere. Other EEG findings were as follows:
All patients were clinically seizure-free by study design. Thirty patients (60%) were weaned off ASMs without seizure recurrence.
Advertisement
Regarding the unoperated hemisphere:
Regarding the disconnected hemisphere:
Dr. Moosa highlights several key takeaways from the analysis of this series:
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits