Findings undercut perceptions of radial artery as second conduit of choice
Are radial artery (RA) grafts superior to saphenous vein (SV) grafts in terms of improving long-term survival for patients undergoing coronary artery bypass grafting (CABG)?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
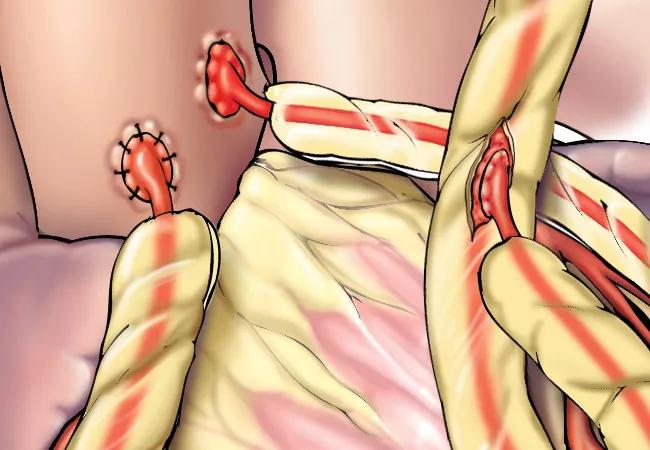
A post hoc analysis of the largest randomized, controlled, multicenter clinical study to date comparing these graft types as second conduits (to supplement a left internal thoracic artery [ITA] bypass to the left anterior descending artery) found similar mortality outcomes between the two options.
“We showed that there was no difference in patient survival between RA and SV grafts and that the survival curves actually near perfectly overlapped,” says Cleveland Clinic cardiothoracic surgeon Faisal Bakaeen, MD, a co-author of the analysis, published as a research letter in Circulation (2022;146:1323-1325). “If your goal is to influence survival, using the RA is unlikely to affect it.”
The analysis was an extension of a large Department of Veterans Affairs (VA) study from more than a decade ago (JAMA. 2011;305:167-174) that compared the two graft types in patients undergoing first-time elective CABG at 11 VA medical centers. The left ITA was used preferentially to graft the left anterior descending coronary artery whenever possible; the best remaining recipient vessel was randomized to an RA graft or an SV graft.
The initial study report showed no difference in graft patency between the two conduits at 12 months after CABG. Since SV graft failure generally occurs between postoperative years 5 and 10, the researchers decided to follow the same patients from randomization to death or Feb. 15, 2021 — whichever was earlier.
Of the study’s 733 participants, 726 consented to database follow-up and were included in the analysis. Median survival was comparable between patients who received an SV graft (14.6 years) and those who received an RA graft (14.2 years) (P = 0.89).
Advertisement
Survival rates still did not differ between the groups after adjustment for various prespecified demographic and clinic variables, and post hoc subgroup analyses found no survival differences between the graft types for any subgroup examined.
“No randomized trial has demonstrated a survival advantage for either RA or SV grafts,” says Dr. Bakaeen.
Observational studies, on the other hand, have suggested reduced all-cause mortality with RA grafting. Dr. Bakaeen suspects these findings may have been influenced by selection bias and surgeon preference and experience, which limits their robustness and generalizability.
“Our VA study reflects real-world experience of multiple surgeons in multiple medical centers,” he says. “Theoretically, you could argue that relative lack of surgeon experience is why RA grafting was nonsuperior in the VA study. However, the study’s perioperative mortality and graft patency rates at one week and one year compare favorably with those of other studies. Graft patency at one year was 89% in both conduit groups. This is comparable to rates achieved by surgeons known for excellent CABG outcomes and is a testament to the skill of cardiac surgeons in the VA system.”
Dr. Bakaeen and co-authors did not present long-term patency data because such data had not been collected in the VA database in a systematic way. “We felt that incomplete data would affect the quality of our conclusions,” he explains.
Lack of complete data during the years of follow-up also led the authors to forgo evaluating the effect of SV or RA grafts on endpoints such as myocardial infarction, heart failure, angina and quality of life. The effect of graft choice on these endpoints remains uncertain.
Advertisement
“No difference in mortality over time doesn’t rule out a possible advantage in these other endpoints, but available patency data suggest outcomes are unlikely to differ,” Dr. Bakaeen says.
While the new analysis of the VA study adds to the evidence base on bypass graft choice, information on certain patient populations remains limited. One group is women, since the majority of patients in the VA study were men.
Another group is individuals with compromised heart function. “As in other published studies comparing RA and SV grafts, most participants in the VA study had normal cardiac function,” Dr. Bakaeen notes. “We don’t know how outcomes would translate in patients with heart failure and left ventricular dysfunction.”
Additionally, only a small share of patients screened for most studies ultimately were enrolled, because a sizable percentage did not have adequate collateral circulation to permit safe harvest of their RA. In addition, some patients did not have a suitable target vessel with 70% or greater stenosis, which was a criterion of the VA study.
While the ITA remains the gold standard graft for CABG, a 2021 joint guideline on coronary artery revascularization (J Am Coll Cardiol. 2022;79:e21-e129) gave RA grafts a class I recommendation as the choice for second conduit. Dr. Bakaeen agrees with colleagues who challenged this decision for a lack of robust supporting evidence.
“Our data say it is premature to make the RA graft standard of care, since it can only be used in certain qualified scenarios and ideally by surgeons experienced in its use,” he says.
Advertisement
Until more information on superiority comes to light, Dr. Bakaeen recommends that surgeons adhere to proven methods and what works best in their hands. “We have demonstrated that use of a second ITA is associated with improved survival,” he says. “If you are a surgeon who achieves excellent results with arterial grafts using a second ITA or an RA, you should continue this practice in patients who are likely to benefit from potential longevity associated with use of these grafts. We believe a surgeon’s skill and judgment are important modifiers of short- and long-term outcomes.”
Advertisement
Advertisement

BITA grafts themselves are rarely to blame, and outcomes can be good

Two cardiac surgeons explain Cleveland Clinic’s philosophy of maximizing arterial graft use

Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity

Study indicates lower in-hospital mortality and better long-term survival

How Cleveland Clinic supported an alliance hospital to improve early extubation practices

Why and how we’re using robotic assistance for qualifying CABG candidates

Innovative approach to the procedure can yield significant relief in complex cases

A scannable recap of our latest data in these clinical areas