Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity
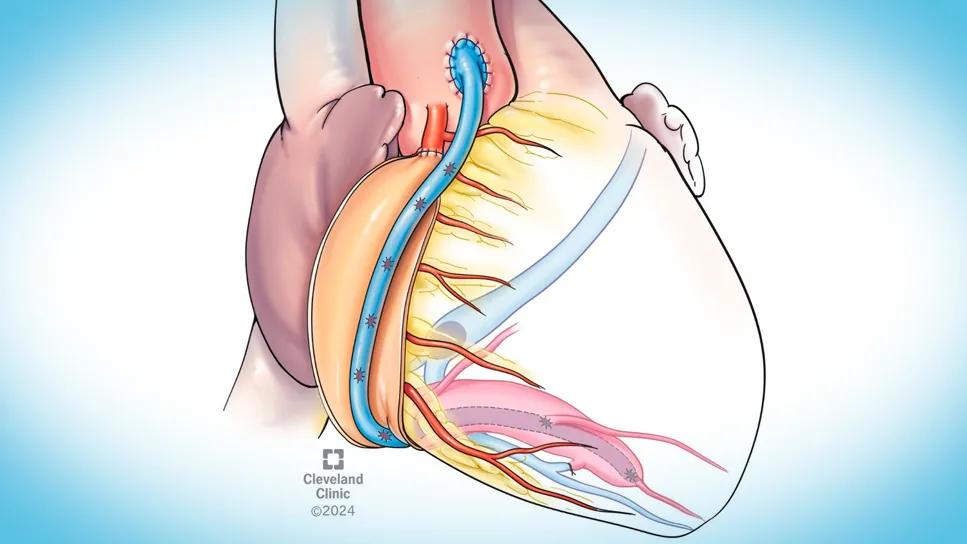
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d0cc53ca-7bcf-4858-8210-f3f7b8e2e4df/25-HVI-6054558-CQD-feature)
illustrated heart with a graft and visible blood vessels
In early 2024, a 61-year-old male physician came to Cleveland Clinic from out of state for an opinion on treatment of a right coronary artery aneurysm (CAA) with a fistula to the coronary sinus. Despite minimal symptoms, periodic imaging tests performed since 2022 indicated dilation of the right ventricle. His local doctors had started him on warfarin and said they could do nothing more. He wanted to know whether surgical repair was an option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient was evaluated by cardiologist Nicholas Ruthmann, MD, and cardiothoracic surgeon Faisal Bakaeen, MD. They found him to be an active individual with mild shortness of breath and fatigue on exertion. A review of his coronary CT scans confirmed a right CAA 1.5 cm in diameter (Figure 1). Nuclear imaging tests revealed mild ischemia in the right ventricle. Their concern was that the patient’s right ventricular function would be severely affected over time due to an increase in loading conditions caused by the fistula.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/78d6c5e9-940f-461b-b8ce-06e3ae5305d8/25-HVI-6054558-CQD-inset-fig1)
Figure 1. The patient’s CT showing the right coronary artery aneurysm within the blue tracing.
Treatment risks, options and alternatives were discussed with the patient. Because his left ventricular ejection fraction had dropped to 50%, his right ventricle was dilating, some tricuspid valve regurgitation was evident and mild symptoms were present, Dr. Bakaeen felt it would be reasonable to proceed with surgery.
The patient decided to continue conservative management for the time being. Over the following six months, however, his symptoms progressed, and his right ventricular function became more significantly affected. He recontacted Cleveland Clinic to schedule the surgery.
In late summer 2024, Dr. Bakaeen repaired the aneurysmal distal coronary artery fistula using a surgical technique pioneered at Cleveland Clinic. The steps involved in this novel technique are clearly explained and illustrated in a seven-patient case series reported by Dr. Bakaeen and Cleveland Clinic colleagues in JACC: Case Reports (2022;4:101665).
The patient had an unremarkable recovery and was discharged home six days after surgery. He subsequently resumed his medical practice and reports feeling full of energy. His prognosis is the same as that of a healthy peer.
Advertisement
The incidence of CAA is believed to be between 0.3% and 5.3%. CAA associated with a fistula to the coronary sinus is even more rare.
Most patients with CAA are male. About 50% of patients have coronary artery disease. Other causes include trauma, connective tissue diseases and congenital issues.
“The most common cause may not always be the direct cause,” says Dr. Ruthmann. “However, we do know this patient had moderate coronary artery disease based on a catheterization he underwent in 2023.”
Dr. Ruthmann notes that CAA symptoms tend to be mild, so most such aneurysms are discovered incidentally. “In this patient, a coronary angiogram showed the dilated artery,” he says (Figure 2). “It is possible that as his CAA enlarged, it acted as a capacitance chamber that compromised the circulation to his heart muscle, increasing fatigue and shortness of breath and prompting him to seek an evaluation.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b85623bf-5fcd-450b-ac83-84c7ba18c11e/25-HVI-6054558-CQD-inset-fig2)
Figure 2. The aneurysmal right coronary artery as seen on angiography.
This patient had a small fistula between the right coronary artery and cardiac vein, which increased pressure in the artery as blood flowed into the lower-resistance vessel. This caused the artery to dilate and form an aneurysm. Blood draining from the fistula and vein into the right atrium overloaded the chamber and, subsequently, the right ventricle. Both chambers dilated and weakened. The tricuspid valve was stretched, causing it to become incompetent and leak.
A small CAA without a fistula can be treated medically. “It is reasonable to start these patients on oral anticoagulants in case there is stasis of blood in the aneurysm, which predisposes to thrombus formation,” Dr. Ruthmann explains.
Advertisement
“When a CAA is large, symptomatic, causing complications or clots with embolization, or has a high-risk feature such as a large aneurysm, we are inclined to operate,” Dr. Bakaeen adds. “We perform about five of these CAA repair operations at Cleveland Clinic every year.”
Some centers attempt to close the fistula surgically or with a catheter. “However, locating the fistula can be very difficult and is often impossible with a catheter-based approach,” Dr. Bakaeen notes. “Some operators have described ligating the fistula and leaving the aneurysm, which is a much simpler operation. However, the fistula provides runoff from the aneurysm, and once it is cut off, blood flow in the aneurysm slows down. This further increases the risk of stasis clot formation. Although anticoagulation is mandatory, it does not guarantee protection against a large and fatal thrombus or embolism.”
Surgical repair of CAAs provides excellent outcomes, as evidenced by a retrospective review of 458 patients treated at Cleveland Clinic with either medical, interventional or surgical management (Open Heart. 2021;8[1]:e001440). Surgically eliminating the aneurysm precludes the risk of clot formation and aneurysm growth and rupture.
“In this patient, we took the section of right coronary artery most proximal to the aorta and oversewed it, creating a cul-de-sac of blood to feed the tiny branches that emerge at this location,” Dr. Bakaeen explains. “Then we used the vein to create eight bypasses, ensuring every meaningful branch to the right ventricle would have an adequate blood supply. Sacrificing these coronary branches would have caused arrhythmias that could have been fatal.” Key aspects of the operation are illustrated in Figure 3.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3cf408de-4de3-41cb-a794-728133a3839c/25-HVI-6054558-CQD-inset-fig3)
Figure 3. The aneurysmal right coronary artery (RCA) was fileted — i.e., incised lengthwise and laid open (1). A saphenous vein harvested endoscopically from the leg was laid inside the RCA and attached sequentially with end-to-side anastomoses (2) to all significant side branches, creating eight bypasses (two on the back of the heart are not visible in this illustration). A cul-de-sac was created in the healthy section of RCA coming off the aorta (3) to secure an adequate blood supply to the early RCA branches. The vein graft was taken off the aorta (4) and this proximal anastomosis became the new blood inflow to the rest of the right side of the heart. Additionally, the fistula was ligated (5).
The surgery proved to be an elegant anatomic solution to a complex problem. “Removing the fistula eliminated the extra volume of blood that had caused the right ventricle to dilate,” Dr. Bakaeen notes. “As a result, the patient’s right ventricle reverted to its normal shape and now functions normally. Moreover, the tricuspid valve no longer leaks.”
Advertisement
Advertisement
BITA grafts themselves are rarely to blame, and outcomes can be good
Two cardiac surgeons explain Cleveland Clinic’s philosophy of maximizing arterial graft use
Study indicates lower in-hospital mortality and better long-term survival
How Cleveland Clinic supported an alliance hospital to improve early extubation practices
Why and how we’re using robotic assistance for qualifying CABG candidates
Findings undercut perceptions of radial artery as second conduit of choice
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing
5 biggest changes according to Cleveland Clinic experts