Restoring sensation following mastectomy
A 62-year-old survivor of triple-negative breast cancer reports very little sensation in her reconstructed breasts. Previously, the patient had a double mastectomy and implant-based reconstruction. The patient states she often experiences tightness and pulling in her chest, and that the breasts are usually cold to the touch. Surgery to replace the implants did little to restore sensation. What options remain for this patient?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Breast cancer can take a physical and psychological toll on patients — and these consequences may be somewhat mitigated by breast reconstruction. Though reconstruction itself is not novel, media attention has mainstreamed concern about hypoesthesia following mastectomy and reconstruction.
“We find it’s much more common for patients to ask about if and when they should expect sensation to return after reconstruction,” states Risal Djohan, MD, Vice Chair of the Department of Plastic Surgery at Cleveland Clinic. “Following breast reconstruction, the return of sensation is unpredictable. Depending on the degree of cutting during mastectomy, sensation may regenerate after a recovery period for some patients, but for others, sensation may never return.”
Although there may be more than one donor site option for autologous breast reconstruction using nerve graft and conduit, the abdominal site is used most commonly. In procedures that include a deep inferior epigastric perforator (DIEP) flap, a sensory nerve supplying the donor flap is isolated, preserved and coapted to the transected intercostal nerve, which is usually removed along with the mastectomy. When Dr. Djohan performs reconstruction using a DIEP flap, he will also look for the nerve segment in the chest and the DIEP flap for potential reconstructions. A nerve graft reconnects each nerve end for a tension-free coaptation, while the conduit protects the coaptation.
According to Dr. Djohan, his current operative technique includes marking and dissecting the DIEP flap, taking care to identify abdominal sensory nerves as they exit the abdominal wall and enter the subcutaneous tissues. In order to achieve adequate length, fascial attachments are released. Next, the free end of the abdominal nerve is coapted to the graft, and the conduit is placed around the coaptation. The chest nerve is isolated under the third or fourth rib, and dissected to increase length and mobility. The free end of the intercostal nerve is coapted to the free end of the graft, and a conduit placed around it. Finally, the flap is tailored and inset.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bf21be75-472a-4d1b-b92f-4431138eb54e/19-PSX-6081-Sensate-Breast-Reconstruction_CQD_650x450_2-300x208_jpg)
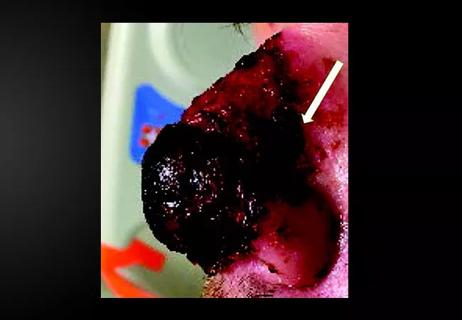
Coaptation of the nerve allograft (blue arrow) and nipple-areolar complex (red arrow).
Coaptation of the nerve allograft (blue arrow) and nipple-areolar complex (red arrow).Finally, the flap is tailored and inset. The procedure is lengthy; however, the innervation only adds roughly 20 minutes per side.
“The length of time until sensation is restored is variable, though we do follow up at standardized time points to evaluate for sensory recovery. We also encourage all our patients to follow our novel rehabilitation protocol for breast sensation, which incorporates various forms of touch and simulation to encourage sensory re-education. The process may take about a year,” notes Dr. Djohan.
In the case above, the patient was a candidate for sensate reconstruction using a DIEP flap. At a two-year follow-up appointment, the patient reports looking and feeling normal. “Sometimes,” she says, “I even forget I had cancer.”
Numerous questions remain about sensate reconstruction, including donor site, timing, technique, patient sensory re-education and long-term outcomes.
“Not all patients are good candidates for DIEP reconstruction. Pre-mastectomy breast size, adipose and skin availability, time in surgery and costs are all considerations. We are exploring additional options for patients that might need them,” says Dr. Djohan.
In 2019, Dr. Djohan and associates from Cleveland Clinic published a review of established targets for autologous flap neurotization, targets that have been used for nonbreast neurotization, and possible targets that have not yet described in the context of neurotization. Targets that have been used for breast neurotization include flaps from the DIEP/transverse rectus abdominis muscle, latissimus dorsi, as well as the superior and inferior gluteal artery perforators. The anterolateral thigh and the tensor fascia lata flaps have been used for neurotization in nonbreast tissue, although uncommonly. There are many other potential targets for autologous sensate breast reconstruction that have yet to be described in the literature, including the lateral thigh, transverse myocutaneoues gracilis, medial circumflex femoral artery perforator, posterior medial thigh, profunda artery perforator, lumbar artery perforator, and Ruben’s fat pad.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9c1cbda3-243a-4cb0-9aa3-b66a29061ed5/19-PSX-6081-Sensate-Breast-Reconstruction_inset_Figure-1-295x300_jpg)
Coaptation of the nerve allograft (blue arrow) and nipple-areolar complex (red arrow).
“Additionally, since not all patients are candidates for autologous reconstruction, we now perform sensate implant-based reconstruction using cadaveric nerve grants. Our preliminary outcomes from this technique are promising, suggesting that sensation is restored to the nipple-areolar complex,” says Dr. Djohan.
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair