Flaps, blebs and other surgical options
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Judging by the discussion at retina conferences, you might get the impression that there’s an epidemic of nonclosing macular holes. However, the closure rate of macular holes is actually very good.
Some macular holes close spontaneously (4%-11.5%) — especially when they’re smaller than 250 microns. According to a 2019 meta-analysis, up to one in 10 of these smaller holes can close on their own. They are more likely to close if they have a bridging membrane and when any remaining traction is released.
In addition, the closure rate of macular holes after internal limiting membrane (ILM) peeling is 90%-97%. At Cleveland Clinic Cole Eye Institute, the closure rate is closer to 98%.
An ILM peel with gas is effective for primary closure of most holes, especially when the hole has been there a short time. This is true whether or not you incorporate postoperative face-down positioning. A 2023 review found no definitive benefit for face-down positioning. However, according to the American Society of Retina Specialists’ Preferences and Trends Survey, 95% of U.S. retina specialists still recommend it for one day, three days, five days or longer postop.
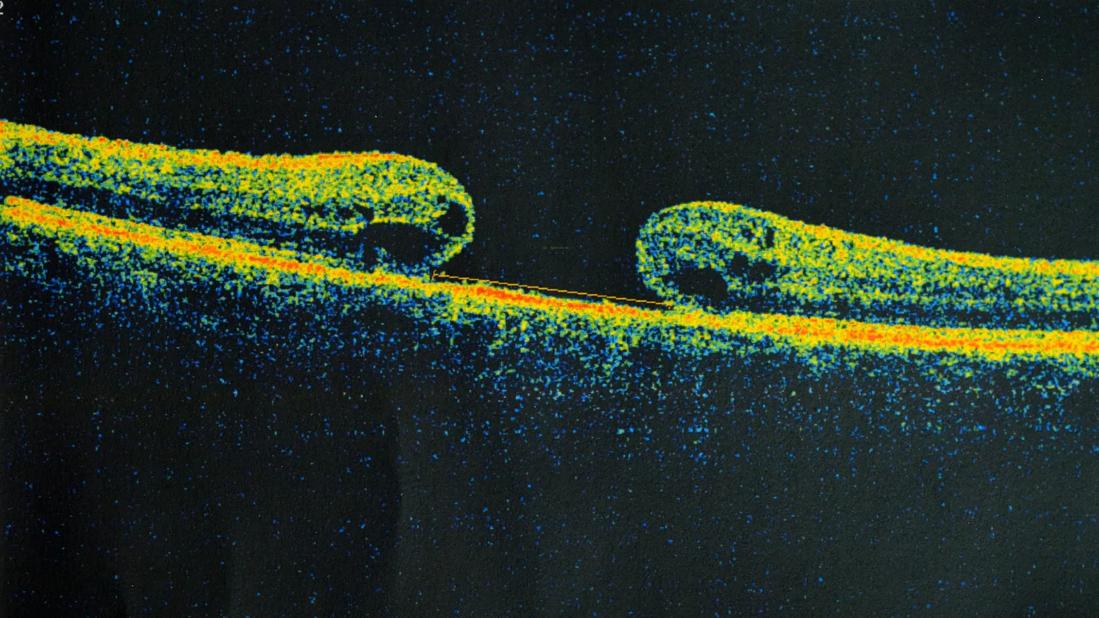
Following an ILM peel, the macular hole can close, either with or without some resolution of the foveal contour and restoration of the ellipsoid zone. Otherwise, you have either a refractory hole that didn’t close after surgery or a type 2 closure (a flat-edged hole, which leaves a central visual field defect).
What should you do when a patient is refractory to primary repair, or has a very large hole or super-high myopia, or has a macular hole in association with retinal detachment? There are a few options.
Advertisement
There are scaffold-based techniques, which include:
There also are manipulation-based techniques, which include:
The inverted ILM flap technique has become quite popular thanks to a number of papers that have been published since 2008. For an inverted ILM flap, you can leave a very large flap or truncate the flap with a cutter, as shown in this video.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_gvskxmqn/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Inverted ILM flap technique to repair a macular hole
When truncating the flap, be careful not to remove the whole thing, which can happen easily. In the video, intraoperative OCT shows that the flap is still attached and that there’s a nice scaffold for the hole to close around. Then we see a slow, gentle air-fluid exchange on the nasal side of the nerve, leaving the flap in position.
A number of inverted ILM flap surgical techniques have been described, but all involve making sure you have a posterior hyaloid detachment (using steroid staining) and ILM staining (with trypan blue, brilliant blue or indocyanine green). The ILM flap techniques that have been used include:
All of these techniques try to increase the closure rate of refractory macular holes.
Advertisement
A 2018 paper compared the inverted flap technique with putting ILM material into the macular hole. The paper reported that the inverted flap technique produced better recovery of the outer retinal layers, better recovery of the external limiting membrane, and improved foveal shape. While there can be complications, the flap provides some type of scaffolding that can help larger holes to close and not reopen.
Other techniques that have been described for closing refractory macular holes involve creating a scaffold from another material, such as an amniotic membrane or lens capsule graft, serum or plasma — taking some blood and actually putting it on the macular hole.
For example, you can use a punch to get a round 1 mm amniotic membrane graft. The graft can be placed into the eye with forceps and then positioned subretinally, under the macular hole. That procedure can produce a nice closure with return of the foveal contour. However, sometimes the outcome is anatomically successful yet does not improve visual acuity. For that reason, I question the utility of these other scaffolding procedures.
But what if you don’t have any material to try to close the hole? Maybe you’ve already done a very large peel and don’t have any viable posterior capsule to use. That is what happened to Grewal and Mahmoud in 2016, when they came up with an innovative technique — autologous retinal transplant — while operating on a patient with a refractory macular hole.
They put in perfluoro-n-octane (PFO), used diathermy to mark an area of retina to remove, cut out the piece of retina using vertical scissors, and then applied a broad base of laser around the edges of the retinotomy. Under PFO, they translocated the retinal flap into or on top of the macular hole, followed by a direct oil exchange.
Advertisement
This autologous retinal transplant potentially provides:
There was some secondary vascularization of that autologous flap. On OCTA, you can see some flow within the retina in about a third of eyes after autologous retinal transplant.
However, macular holes still may fail to close after retinal transplant. The flap can migrate or retract, for example. And there can be other complications, such as:
This procedure isn’t easy. Readjusting under PFO is very difficult. If you lose one graft and need to get a second one, you make multiple holes in the retina. You can end up with subretinal perfluorocarbon. A large posterior staphyloma can be challenging too. As such, autologous retinal transplant remains a technique of last resort, when there are no other options for closure, but the patient is motivated to make one last attempt.
Recently, my preferred technique for refractory or large macular holes has been manipulation-based, using subretinal blebs. The blebs allow for mobilization of the hole’s edges, bringing them closer together. Often, I will inject a small PFO bubble to prevent the fluid from refluxing through the hole.
There are many ways to create blebs, including direct subretinal injection with a subretinal needle. A gentler method that has been described involves refluxing fluid with a soft-tip extrusion cannula after you peel the ILM. After creation of the blebs, I will sometimes gently massage the edges of the hole with a flex loop to bring the edges closer together.
Advertisement
Note, however, that the patient sometimes ends up with atrophy of the retinal pigment epithelium where you create the bleb. Although the macular hole may close, the retina can appear generally atrophic and have multiple areas of complete atrophy. A gentle technique with slow injection of fluid into the subretinal space is warranted.
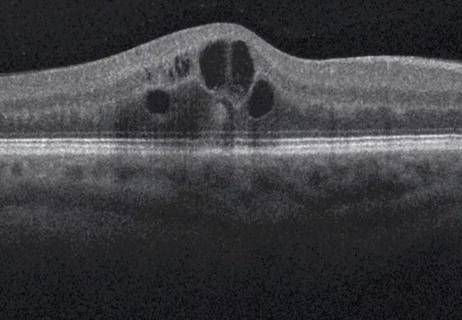
The most difficult cases are those involving a macular hole with a retinal detachment, as seen in this video.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_dm14bw44/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Repairing a macular hole with retinal detachment
Be careful not to inject indocyanine green (ICG) when the retina is detached and a macular hole is wide open. ICG can flow into subretinal space, which is concerning since ICG can be toxic to photoreceptors.
Instead, you can use a bubble of PFO to protect the hole, put in ICG, let it stain the retina, and then remove it. Then use the PFO to hold the retina in place to initiate your flap. Be sure the PFO bubble isn’t small enough to go subretinal through the hole as well.
In the above video, we took out the PFO once we had initiated the flap because it was easier to peel the ILM without the PFO in place. Peeling the ILM with a detached retina is challenging. The initial grab of ILM is often difficult as the retina moves away from you. The key is being patient.
Sometimes, videos of peels make the process look quick and easy. The peel shown above took about 20 minutes. (The video is in real speed but doesn’t show all the attempts to take off the membrane.) With some patience, the ILM came off nicely, and the macular hole eventually closed.
Dr. Sharma is a vitreoretinal and uveitis specialist at Cleveland Clinic Cole Eye Institute. This article was based on his presentation at the 2024 Cole Eye Institute Retina Summit.
Advertisement

Study identifies factors that may predict vision outcomes in diabetic macular edema
Greater central subfield thickness and better visual acuity at baseline are associated with longer time to resolution

Can a single subretinal injection provide effective treatment?

New insights on effectiveness in patients previously treated with other anti-VEGF drugs

Evidence mounts that these diabetes and obesity drugs may protect eyes, not endanger them

CFH gene triggers the eye disease in white patients but not Black patients

A primer on sustained release options

Study explores association between sleep aid and eye disease