Randomized trial demonstrates noninferiority to therapist-led training

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b2993078-7291-4117-ad57-4a8d1ea342af/23-NEU-4201372-CQD-Hero-967x544-1_jpg)
illustration of two people taking a gait test wearing augmented reality headsets
Dual-task training has been shown to enhance gait performance in people with Parkinson’s disease (PD), but it is underutilized due to barriers to implementation. Now a novel digital therapeutic approach to dual-task training (DTT) using augmented reality has shown noninferiority to traditional DTT in improving gait performance in a randomized controlled trial in this population. The findings, published by Cleveland Clinic researchers in Neurorehabilitation and Neural Repair (Epub 2023 Jul 19), promise to help expand the gait benefits of dual-task training to more patients with PD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“To our knowledge, this is the first digital therapeutic for Parkinson’s disease that has undergone rigorous evaluation against an accepted intervention in a randomized controlled trial,” says lead investigator Jay Alberts, PhD, Vice Chair of Innovation in Cleveland Clinic’s Neurological Institute and staff in the Department of Biomedical Engineering. “These findings suggest that we can address barriers to wider use of dual-task training. This intervention can serve as a model for future digital therapeutics designed to ameliorate the effects of Parkinson’s disease.”
The intervention he refers to is the Dual-task Augmented Reality Treatment (DART) platform, which his Cleveland Clinic team developed to simultaneously deliver a validated DTT intervention while objectively measuring gait and cognitive performance during the training. Users of the DART platform wear a Microsoft HoloLens2 augmented reality headset while completing a series of tasks designed to engage the body and mind simultaneously. The headset projects digital objects in the ambulating user’s path while challenging them with cognitive tasks, and the user’s gait function and responses to the challenges are evaluated in real time.
Development of the DART platform, which can generate more than 230 combinations of DTT activities, was recently described by the team in Sensors (Basel) (2022 Nov 12;22[22]:8756).
“The platform merges the real and digital worlds in a way that creates a unique enhanced environment well suited to delivering dual-task training scenarios that facilitate rehabilitation training,” Dr. Alberts explains.
Advertisement
Development of the platform was prompted by persistent challenges in managing postural instability and gait dysfunction in people with PD, as nearly 80% of this population falls at least once per year. The fall risk is particularly pronounced when a person with PD performs an attention-demanding cognitive task while moving (i.e., dual tasking).
This gave rise to DTT, which has been shown in randomized trials over the past decade to improve the performance of patients with PD in gait, balance, physical activity and dual-task cognitive ability. Despite this effectiveness, DTT is not widely used because of the time and resources required to personalize a program for patients, monitor patient progress and keep the intervention engaging over time.
“Traditional dual-task training requires one-on-one attention from a physical therapist throughout a patient’s training session, which places clear limits on how much training can be offered,” Dr. Alberts notes. “This made it a natural candidate for a potential digital therapeutic intervention.”
His team modeled the DART platform after an eight-week therapist-led DTT intervention that demonstrated improvements in single-and dual-task gait velocity in a randomized trial among individuals with PD (Parkinsonism Relat Disord. 2019;64:280-285).
Under the platform, a physical therapist creates a patient-specific DART treatment schedule, which takes five to seven minutes of the therapist’s time. A DART session consists of eight to 12 dual-task modules pairing a motor task with a cognitive task. Each task can be adjusted for difficulty, and patients progress through modules at their own pace, repeating instructions as needed.
Advertisement
Instead of a human therapist, the DART platform uses a digital avatar that appears in the headset user’s field of view and demonstrates exercises and movements while the user hears instructions through the headset. All the while, the headset tracks the user’s movements and responses, collecting objective data that are later displayed on a digital tablet device for clinicians to review and use to design future sessions (see Figure below).
“A digital platform that completes some of the tasks of the traditional DTT intervention, down to collecting tiny alterations in someone’s stride, can help us standardize and implement DTT,” Dr. Alberts says. “We conducted the current trial to determine whether the DART platform could produce improvements in gait and postural stability similar to those with therapist-directed DTT.”
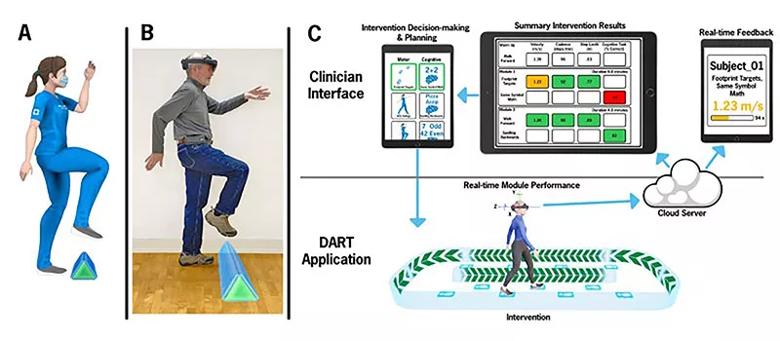
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c85268c9-8b5b-4e21-9e45-4b8f3245bedd/23-NEU-4201372-CQD-Inset-800x350-1_jpg)
Figure. Overview of the DART platform. (A) An avatar demonstrates physical therapy exercises that the platform user can see while wearing the augmented reality headset. (B) A headset-wearing user follows along with the program. The object on the floor is a hologram obstacle visible only to the headset wearer. (C) The headset records and analyzes user progress for clinician review on tablet device.
Study participants were Cleveland Clinic patients with PD who had postural instability and gait dysfunction. Patients were randomized in a single-blind manner to 16 therapeutic sessions over eight weeks involving either traditional therapist-led DTT as used in the earlier randomized trial by Dr. Alberts’ group (Parkinsonism Relat Disord. 2019;64:280-285) or DTT using the DART platform.
Advertisement
Primary outcomes were the following measures, assessed by a blinded assessor and blinded technician at baseline, end of therapy and eight weeks after the end of therapy:
Of 51 patients randomized, four withdrew before the end of treatment (two from each treatment group), leaving 47 patients in the study analysis (22 in the traditional DTT group and 25 in the DART group). All withdrawals were for reasons unrelated to the study. The two groups were comparable on demographic measures.
While clinical measures of PD symptoms held steady throughout the study period across the overall cohort, both treatment groups demonstrated a significant increase in various gait measures by the end of treatment, and improvements in gait parameters in the DART group were noninferior to those in the traditional DTT group under the majority of conditions.
The significant improvements were specifically seen in gait velocity, cadence and step length during single- and multiple dual-task conditions and were largely maintained through eight weeks after the end of therapy.
“In all conditions assessed, improvements in gait speed surpassed the thresholds for small to moderate clinically important differences in gait speed for people with Parkinson’s disease, which suggests that the improvements with both types of DTT intervention were clinically meaningful,” Dr. Alberts notes.
Advertisement
Patients in the DART group gave the DART platform a mean usability score of “good to excellent.” Additionally, the high study retention rate (withdrawal of less than 10% in each group) suggests that adherence would not be an obstacle to DART platform implementation.
The researchers are currently preparing an FDA submission for use of the DART platform as a digital therapeutic in this setting. They emphasize that the platform is not meant to supplant the role of physical therapists in DTT for patients with PD but to permit a single physical therapist to offer DTT and monitoring to more patients, enabling more widespread use of DTT.
“People diagnosed with Parkinson’s disease often balance physical therapy, new medications and specialist appointments with their lives and families, which can be overwhelming,” Dr. Alberts concludes. “Our goal is to make dual-task training more accessible, removing one more obstacle for patients who want to improve their daily lives.”
Advertisement
Various AR approaches affect symptom frequency and duration differently
Dopamine agonist performs in patients with early stage and advanced disease
Early assessment could affect clinical decision making
Systems genetics approach sets stage for lab testing of simvastatin and other candidate drugs
Study aims to inform an enhanced approach to exercise as medicine
New tool for general neurologists aims to streamline differential diagnosis
When and how a multidisciplinary palliative care clinic can fill unmet needs for this population
Research project will leverage insights into neural circuits to advance DBS technology