Trial results point the way to further investigation
Approved for treating myelodysplastic syndrome (MDS) and leukemia, the hypomethylating agent azacitidine has been investigated as a treatment for relapsed or refractory multiple myeloma (RRMM) patients. The plasticity of multiple myeloma, characterized by frequent epigenetic changes, makes it challenging to treat. Patients eventually become resistant to treatment which is driven by DNA hypo- and hypermethylation. Myeloma patients who are refractory to proteasome inhibitors, immunomodulatory drugs and anti-CD 38 antibodies have a median survival of six months, so there is a compelling need for more effective treatments.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
After in vitro testing of azacitidine showed positive results, Cleveland Clinic researchers conducted one of the first trials to study azacitidine in RRMM patients. “We are trying to come up with better and novel strategies to address treatment resistance. As a DNA methylation inhibitor, azacitidine can reverse epigenetic changes and promote better treatment efficacy,” says Jack Khouri, MD, a hematologist/oncologist in the Department of Hematologic Oncology and Blood Disorders at Cleveland Clinic Cancer Center.
The researchers developed a regimen combining a low dose of azacitidine with lenalidomide and dexamethasone to assess tolerability and whether azacitidine could restore sensitivity to lenalidomide. The goal was to reach epigenetically active levels eight times in 28 days with a lower dose of azacitidine than the standard of seven consecutive doses used in myeloid neoplasms to potentially reduce bone marrow toxicity and enable safe combination with lenalidomide. Azacitidine was escalated from 30 mg/m2 once a week up to a predefined maximum of 50 mg/m2 twice a week, in combination with GFR-adjusted lenalidomide (≥ 60 mL/min: 25 mg, 3059 mL/min: 10 mg) from day 1 to 21 every 28 days, and dexamethasone 40 mg once a week. A limited expansion study to 23 days at the highest tolerated dose followed.
The trial cohort included 42 RRMM patients (41 who could be evaluated) with an average age of 62.5, who were treated with a median of five prior lines of therapy. Most (34, 81%) were refractory to lenalidomide and/or pomalidomide.
Advertisement
Like other RRMM treatment regimens, the adverse effects were mainly hematologic: 28 patients (67%) experienced Grade 3 or 4 adverse events including neutropenia and thrombocytopenia.
At a median follow up time of 60.2 months, the overall response and clinical benefit response rates were 22 and 32%, respectively, with four very good partial responses (10%), five partial responses (12%), and four minor responses (10%). The median progression-free survival was 3.1 months, median time to progression 2.7 months and median overall survival 18.6 months. “Azacitidine can help overcome the refractory rate, but only at a low rate,” says Dr. Khouri.
The full results are published in Seminars in Hematology.
The researchers conducted a detailed analysis of patient data to assess how levels of the azacytidine-inactivating enzyme cytidine deaminase (CDA) affects treatment response; they found that low plasma CDA levels are associated with greater clinical benefit. This may suggest potential strategies for increasing the efficacy of azacitidine, including dose modification and concurrent administration of CDA inhibitors to enhance drug exposure.
“Now that we have learned more about azacitidine and its potential role in myeloma, we can use this knowledge in future trials to enhance its efficacy in different combination strategies as well,” says Dr. Khouri. A follow-up trial is under consideration, while an ongoing study is evaluating azacitidine in combination with the anti-CD38 antibody daratumumab in patients with RRMM who have already been treated with daratumumab.
Advertisement
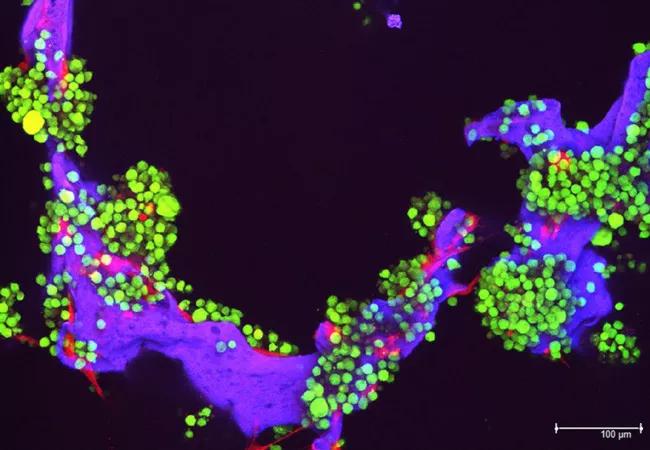
Image: Myeloma tumor cells (in green) and bone cells (red) growing on a scaffold made of silk protein (purple), which is designed to resemble bone material. Source: National Cancer Institute Visuals Online.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient