Survey results reveal need for further education

By Erica Newlin, MD, and Chad Michener, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Preliminary results from research conducted at Cleveland Clinic confirms the need for further education of gynecologic oncologists on the roles of palliative care beyond hospice. When we think of palliative care as synonymous with hospice care, as opposed to symptom management, patients may pay the price, experiencing pain and treatment-related morbidities while undergoing aggressive treatment or surgeries toward the end of their lives. Earlier referral to palliative medicine services can make the transition to hospice and goals of care easier for patients and their families.
Previous studies note the frequent use of aggressive measures at the end of life. In gynecologic oncology literature, a retrospective chart review examining interventions in the last six months of life found that 71% of patients underwent chemotherapy and 59% underwent procedures. One study looking particularly at ovarian cancer, found that 50% of patients underwent a form of “aggressive care” in the last 30 days of life. Analysis of SEER data found that slightly more than one-third of older women dying with ovarian cancer did not access hospice care until the last 7 days of life. Another study, expanding to all gynecologic cancer patients who had died, found that 29% were never referred to palliative care referral and 15% were never referred to hospice.
Given multiple studies documenting the lack of timely palliative care referrals, we aimed to explore the barriers to hospice and palliative care enrollment, as perceived by physicians. Our survey was distributed to 1,410 members of the Society of Gynecologic Oncology members. Of those, 176 (12.5%) participated. Among respondents, 60% were female, 58 were part of academic medicine practices, 53% had personal experience with hospice and 87.5% managed chemotherapy. Self-selection bias is a limitation of this study; we assume that respondents likely had an interest in palliative care.
Advertisement
The highest ranked barriers were primarily “physician factors,” which included physician desire to attempt additional lines of chemotherapy and difficulty accurately predicting patient death to within six months. Interestingly, patient factors of non-receptivity by family and patient desire to pursue additional lines of chemotherapy were ranked among the lowest barriers.
When examining the reasons for hospice referral, we did not see a sizable difference in rankings. All factors trended toward the “more important” side of the spectrum. However; pain control and assistance through the dying process were most highly ranked, as expected.
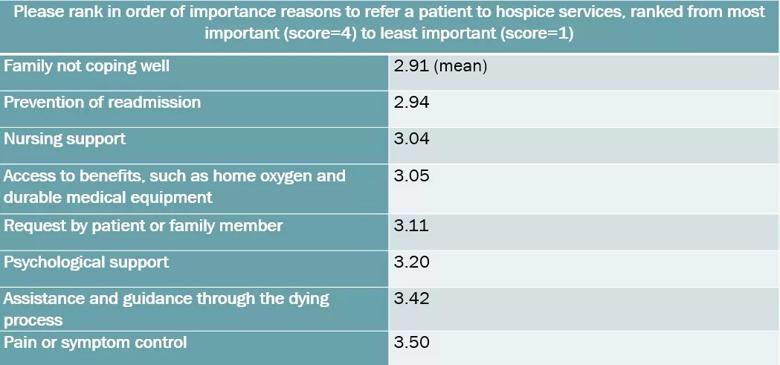
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7894fd15-8612-4cb6-aeab-91bbf8652d5f/table-1_jpg)
Breaking out responses from attending physicians and fellows, attending physicians valued nursing support and prevention of readmission significantly higher. These differences could potentially correlate with the impact of readmissions on reimbursement and hospital rankings, as well as increased experiences with the supplemental support provided by hospice care.
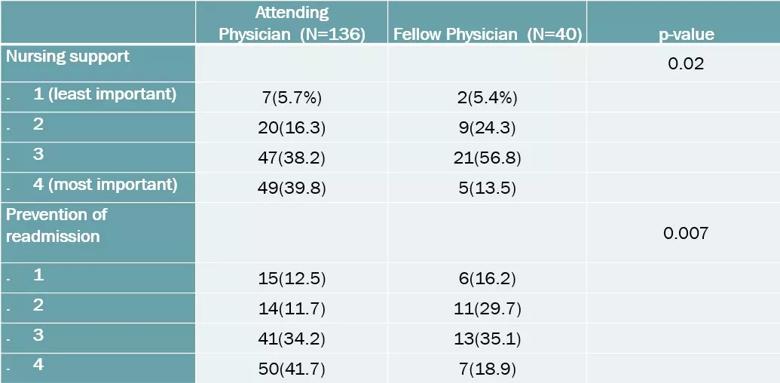
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/84284753-0263-46e3-957b-57ae34613389/table-2_jpg)
When asked specifically about the primary role of palliative care, respondents pointed to pain management (31%), symptom management (29%), hospice transition (22%) and goals of care (18%).
Grouping together goals of care and hospice transition, 40% felt this to be the primary role of palliative care, highlighting a potential trend in late involvement of palliative care services among a significant cohort of responses.
Most respondents strongly disagreed that hospice care hastened patient death. They also tended to disagree that palliative care hindered or interfered with their overall plans of care. More than 85% of respondents felt that gynecologic oncologists develop a unique bond with patients compared to medical or surgical oncologists, and a similar number of respondents view end of life care as an integral part of their practice.
Advertisement
The data again differed between attending physicians and fellows, with fellows more often associating palliative services with pain and symptom management. More attending physicians thought the primary role of palliative medicine at their hospital was to elucidate the goals of care and manage the transition to hospice.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d6fa334-2812-4f8a-a7ba-5328c2770de6/table-3_jpg)
The differences in responses between attending physicians and fellows may stem from changes to medical school curriculum that emphasize palliative care services outside of goals of care and hospice. This difference may also account for the trend of late referrals to palliative medicine services. Alternatively, the differences could also be accounted for by the frequent position of fellows as bystanders in care, as they are still learning the course of the disease.
We are still compiling data on the impact of factors like religious beliefs and the availability of palliative care on the management of patients with gynecologic cancers nearing the end of life. We seek to better understand how we might work better with palliative care and hospice teams to provide the best possible care for patients. This research may ultimately be applied to the development of an educational model outlining the role of palliative care outside the goals of care and hospice transition. Future areas of research may also include patient perspectives about their own struggles with physician management and when they feel would be an appropriate time to receive a palliative medicine referral.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors